Filling out pharmacy claim form is not difficult. Our experts designed our software to really make it intuitive and allow you to fill in any form online. Listed here are steps you will want to take:
Step 1: On this website page, click the orange "Get form now" button.
Step 2: Once you access our pharmacy claim form editing page, you will see all the functions it is possible to take about your document in the top menu.
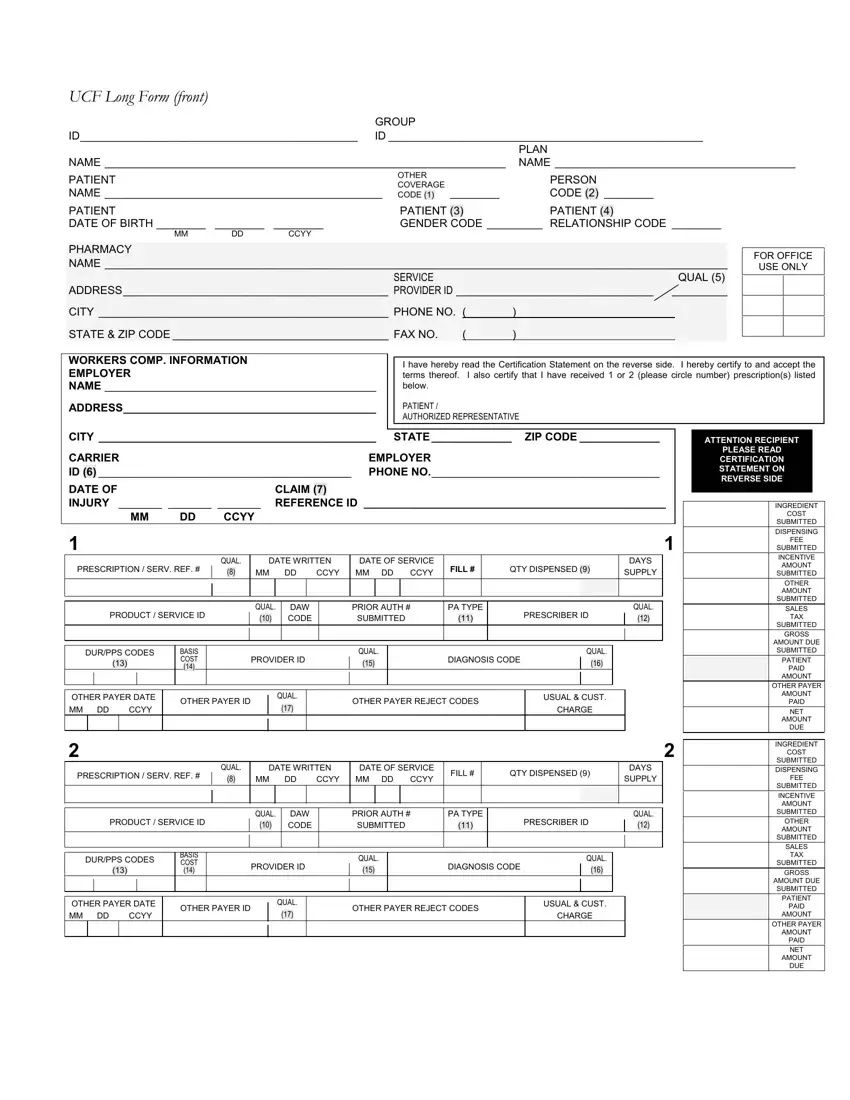
To get the template, provide the content the software will request you to for each of the appropriate segments:
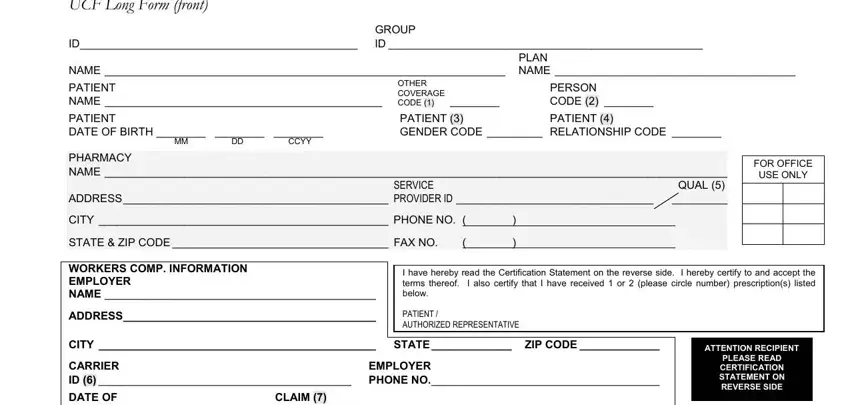
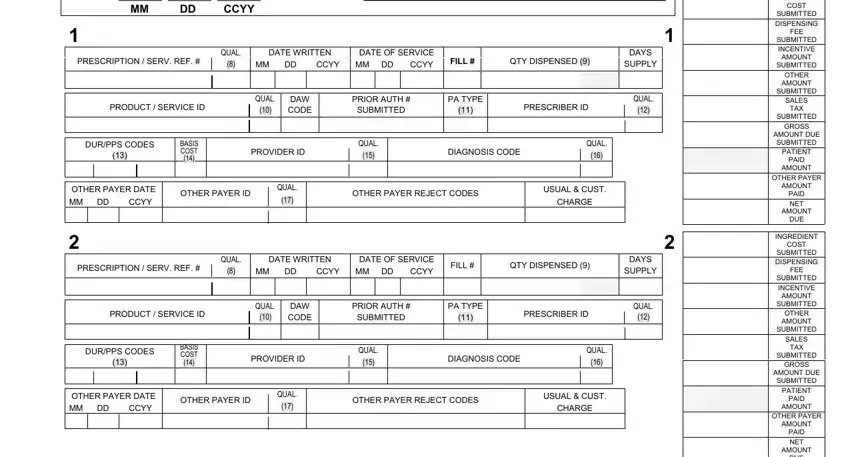
Within the section DATE OF INJURY REFERENCE ID MM, PRESCRIPTION SERV REF, QUAL, DATE WRITTEN, CCYY MM DD, DATE OF SERVICE CCYY, FILL, QTY DISPENSED, PRODUCT SERVICE ID, QUAL, DAW CODE, PRIOR AUTH SUBMITTED, PA TYPE, PRESCRIBER ID, and DURPPS CODES write down the information that the application requires you to do.
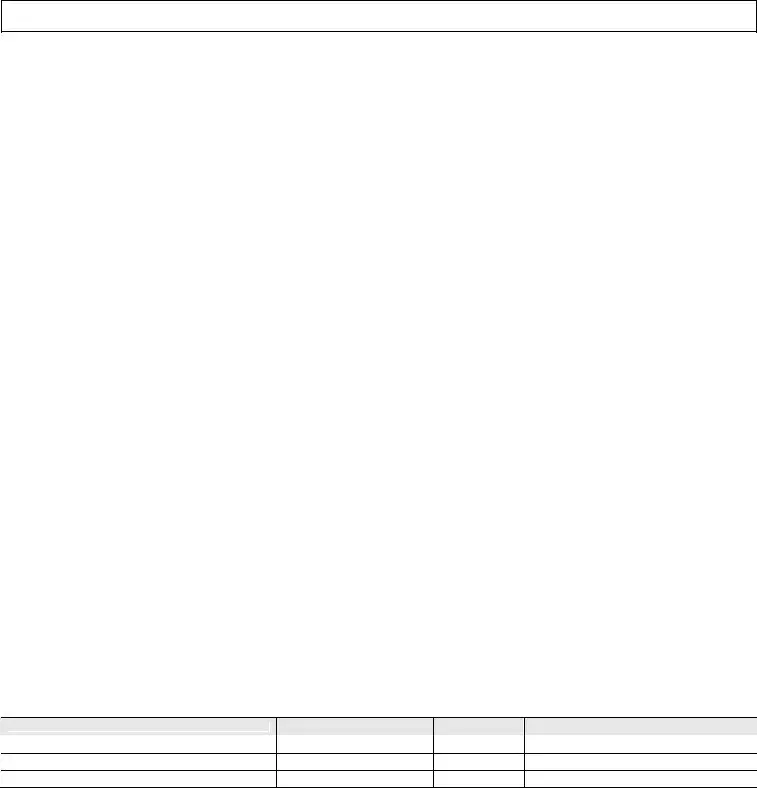
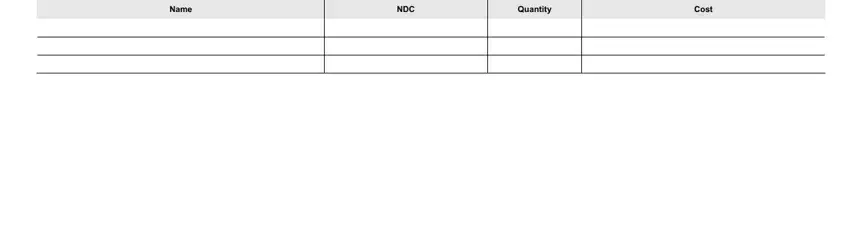
The application will ask you to present certain significant info to effortlessly submit the segment COMPOUND PRESCRIPTIONS LIMIT, Name, NDC, Quantity, and Cost.
Step 3: Press the button "Done". The PDF form is available to be transferred. You can download it to your computer or send it by email.
Step 4: Generate duplicates of the document. This should save you from potential future issues. We don't check or distribute the information you have, thus feel comfortable knowing it's going to be safe.