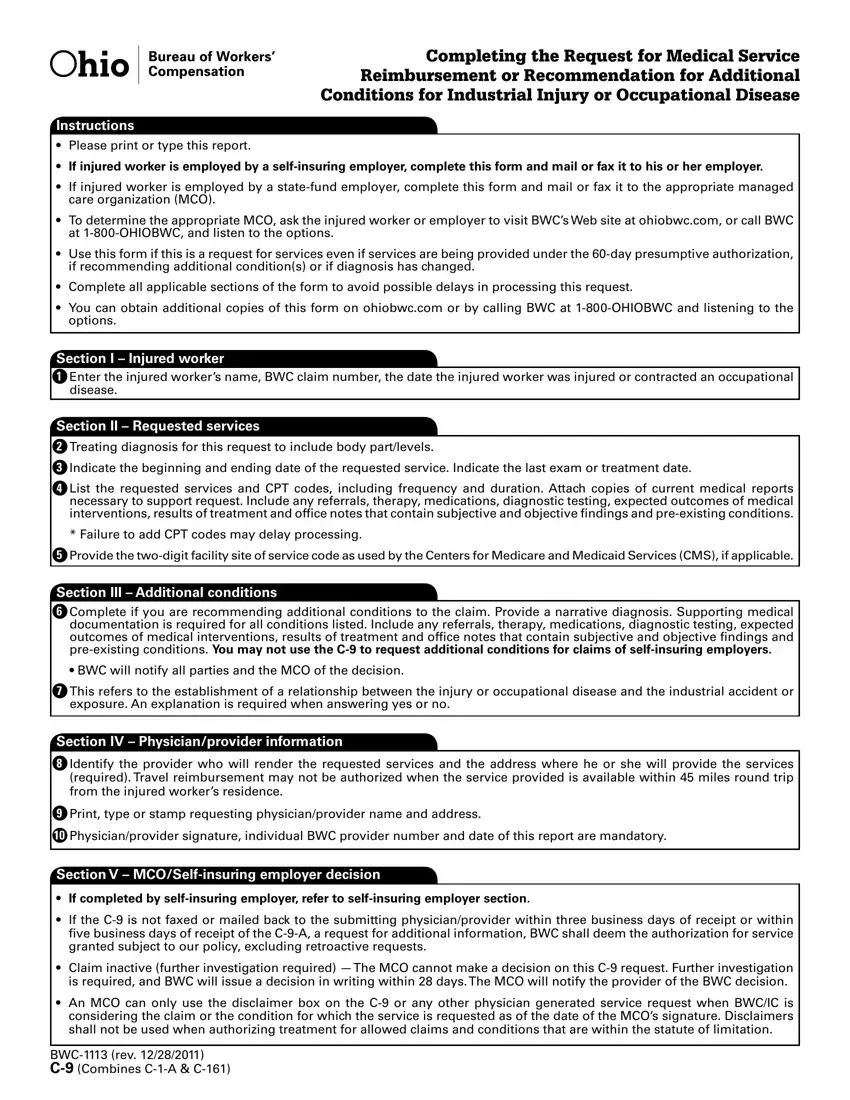
Completing the Request for Medical Service
Reimbursement or Recommendation for Additional
Conditions for Industrial Injury or Occupational Disease
Instructions
•Please print or type this report.
•If injured worker is employed by a self-insuring employer, complete this form and mail or fax it to his or her employer.
•If injured worker is employed by a state-fund employer, complete this form and mail or fax it to the appropriate managed care organization (MCO).
•To determine the appropriate MCO, ask the injured worker or employer to visit BWC’s Web site at ohiobwc.com, or call BWC at 1-800-OHIOBWC, and listen to the options.
•Use this form if this is a request for services even if services are being provided under the 60-day presumptive authorization, if recommending additional condition(s) or if diagnosis has changed.
•Complete all applicable sections of the form to avoid possible delays in processing this request.
•You can obtain additional copies of this form on ohiobwc.com or by calling BWC at 1-800-OHIOBWC and listening to the options.
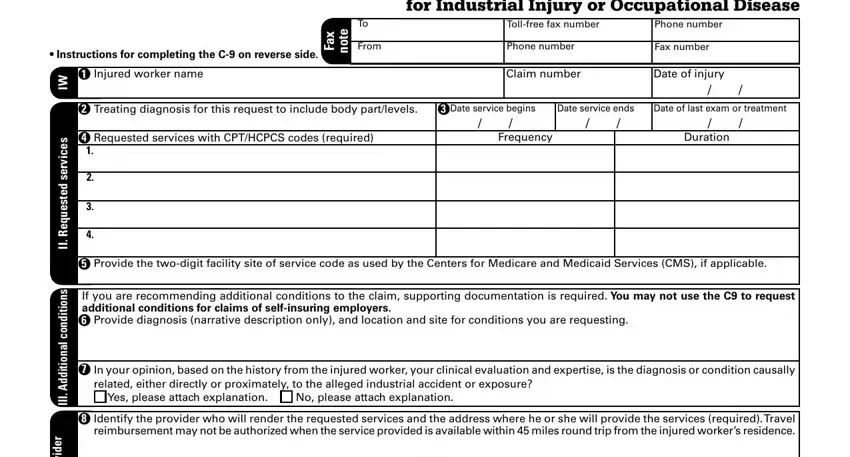
Section I – Injured worker
1Enter the injured worker’s name, BWC claim number, the date the injured worker was injured or contracted an occupational disease.
Section II – Requested services
2Treating diagnosis for this request to include body part/levels.
3Indicate the beginning and ending date of the requested service. Indicate the last exam or treatment date.
4List the requested services and CPT codes, including frequency and duration. Attach copies of current medical reports necessary to support request. Include any referrals, therapy, medications, diagnostic testing, expected outcomes of medical interventions, results of treatment and ofice notes that contain subjective and objective indings and pre-existing conditions.
*Failure to add CPT codes may delay processing.
5Provide the two-digit facility site of service code as used by the Centers for Medicare and Medicaid Services (CMS), if applicable.
Section III – Additional conditions
6Complete if you are recommending additional conditions to the claim. Provide a narrative diagnosis. Supporting medical documentation is required for all conditions listed. Include any referrals, therapy, medications, diagnostic testing, expected outcomes of medical interventions, results of treatment and ofice notes that contain subjective and objective indings and pre-existing conditions. You may not use the C-9 to request additional conditions for claims of self-insuring employers.
• BWC will notify all parties and the MCO of the decision.
7This refers to the establishment of a relationship between the injury or occupational disease and the industrial accident or exposure. An explanation is required when answering yes or no.
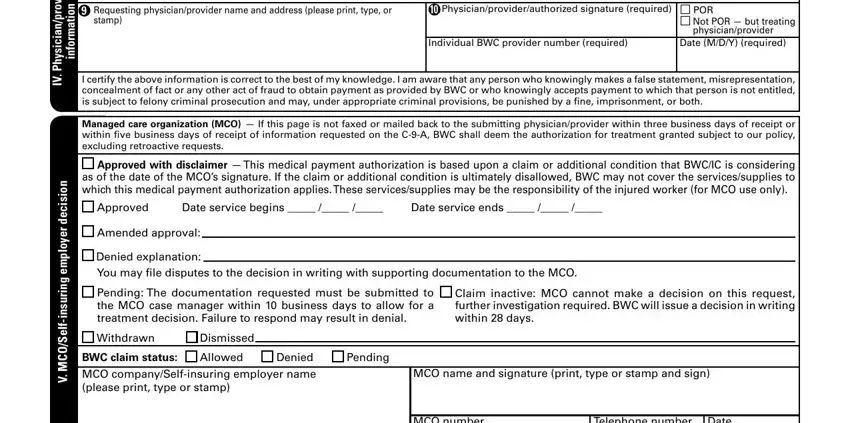
Section IV – Physician/provider information
8Identify the provider who will render the requested services and the address where he or she will provide the services (required). Travel reimbursement may not be authorized when the service provided is available within 45 miles round trip from the injured worker’s residence.
9Print, type or stamp requesting physician/provider name and address.
10Physician/provider signature, individual BWC provider number and date of this report are mandatory.
Section V – MCO/Self-insuring employer decision
•If completed by self-insuring employer, refer to self-insuring employer section.
•If the C-9 is not faxed or mailed back to the submitting physician/provider within three business days of receipt or within ive business days of receipt of the C-9-A, a request for additional information, BWC shall deem the authorization for service granted subject to our policy, excluding retroactive requests.
•Claim inactive (further investigation required) —The MCO cannot make a decision on this C-9 request. Further investigation is required, and BWC will issue a decision in writing within 28 days.The MCO will notify the provider of the BWC decision.
•An MCO can only use the disclaimer box on the C-9 or any other physician generated service request when BWC/IC is considering the claim or the condition for which the service is requested as of the date of the MCO’s signature. Disclaimers shall not be used when authorizing treatment for allowed claims and conditions that are within the statute of limitation.
BWC-1113 (rev. 12/28/2011)
C-9 (Combines C-1-A & C-161)
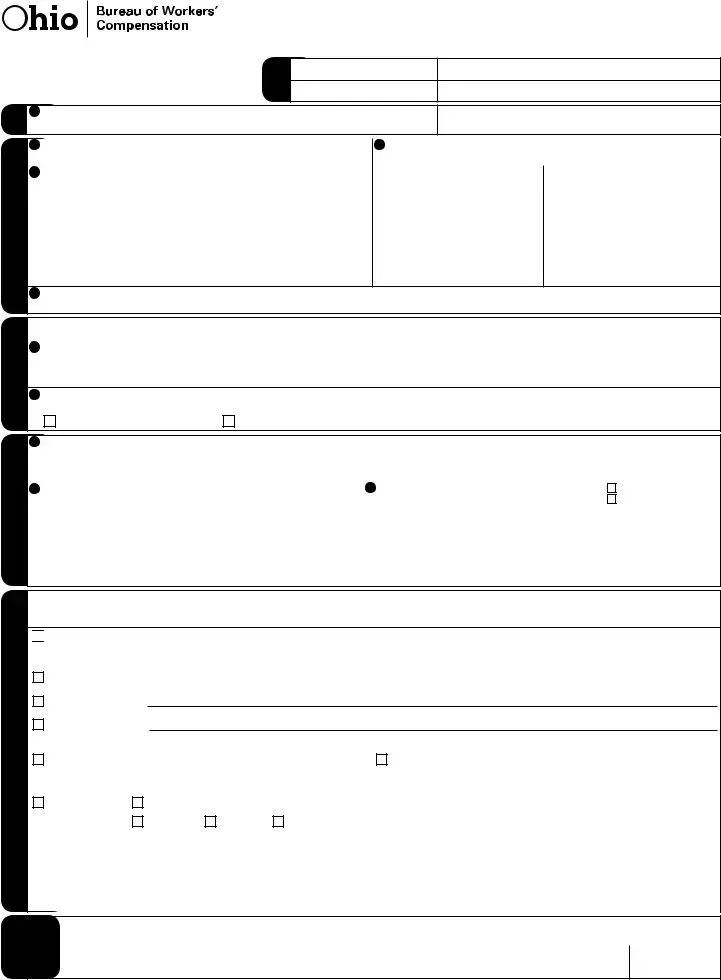
Request for Medical Service Reimbursement or Recommendation for Additional Conditions for Industrial Injury or Occupational Disease
• Instructions for completing the C-9 on reverse side.
Toll-free fax number |
|
Phone number |
|
Phone number |
|
Fax number |
|
Claim number |
|
Date of injury |
|
|
|
|
|
|
|
/ |
/ |
II. Requested services |
III. Additional conditions |
Physician/provider |
information |
IV. |
|
V. MCO/Self-insuring employer decision
2 |
Treating diagnosis for this request to include body part/levels. |
3 Date service begins |
Date service ends |
Date of last exam or treatment |
|
|
/ |
/ |
/ |
/ |
/ |
/ |
4 |
Requested services with CPT/HCPCS codes (required) |
|
Frequency |
|
|
Duration |
|
1. |
|
|
|
|
|
|
|
|
|
|
|
|
|
2. |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
3. |
|
|
|
|
|
|
|
|
|
|
|
|
|
4. |
|
|
|
|
|
|
5Provide the two-digit facility site of service code as used by the Centers for Medicare and Medicaid Services (CMS), if applicable.
If you are recommending additional conditions to the claim, supporting documentation is required. You may not use the C9 to request
additional conditions for claims of self-insuring employers.
6Provide diagnosis (narrative description only), and location and site for conditions you are requesting.
7In your opinion, based on the history from the injured worker, your clinical evaluation and expertise, is the diagnosis or condition causally related, either directly or proximately, to the alleged industrial accident or exposure?
|
Yes, please attach explanation. |
|
No, please attach explanation. |
8Identify the provider who will render the requested services and the address where he or she will provide the services (required).Travel reimbursement may not be authorized when the service provided is available within 45 miles round trip from the injured worker’s residence.
9 |
Requesting physician/provider name and address (please print, type, or |
10 Physician/provider/authorized signature (required) |
POR |
|
stamp) |
|
Not POR — but treating |
|
|
|
physician/provider |
|
|
Individual BWC provider number (required) |
Date (M/D/Y) (required) |
|
|
|
|
I certify the above information is correct to the best of my knowledge. I am aware that any person who knowingly makes a false statement, misrepresentation, concealment of fact or any other act of fraud to obtain payment as provided by BWC or who knowingly accepts payment to which that person is not entitled, is subject to felony criminal prosecution and may, under appropriate criminal provisions, be punished by a ine, imprisonment, or both.
Managed care organization (MCO) — If this page is not faxed or mailed back to the submitting physician/provider within three business days of receipt or within ive business days of receipt of information requested on the C-9-A, BWC shall deem the authorization for treatment granted subject to our policy, excluding retroactive requests.

 Approved with disclaimer — This medical payment authorization is based upon a claim or additional condition that BWC/IC is considering as of the date of the MCO’s signature. If the claim or additional condition is ultimately disallowed, BWC may not cover the services/supplies to which this medical payment authorization applies.These services/supplies may be the responsibility of the injured worker (for MCO use only).
Approved with disclaimer — This medical payment authorization is based upon a claim or additional condition that BWC/IC is considering as of the date of the MCO’s signature. If the claim or additional condition is ultimately disallowed, BWC may not cover the services/supplies to which this medical payment authorization applies.These services/supplies may be the responsibility of the injured worker (for MCO use only).
Approved |
Date service begins _____ /_____ /_____ |
Date service ends _____ /_____ /_____ |
Amended approval:
Denied explanation:
You may ile disputes to the decision in writing with supporting documentation to the MCO.
Pending: The documentation requested must be submitted to |
Claim inactive: MCO cannot make a decision on this request, |
the MCO case manager within 10 business days to allow for a |
further investigation required. BWC will issue a decision in writing |
treatment decision. Failure to respond may result in denial. |
within 28 days. |
|
|
|
|
Withdrawn |
Dismissed |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
BWC claim status: |
Allowed |
Denied |
Pending |
|
|
|
|
|
MCO company/Self-insuring employer name |
|
MCO name and signature (print, type or stamp and sign) |
|
|
(please print, type or stamp) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
MCO number |
Telephone number |
Date |
|
|
|
|
|
|
|
|
( ) |
/ |
/ |
|
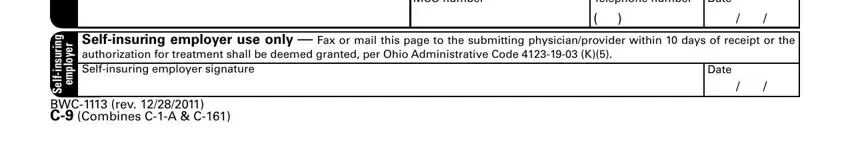
insuring-Self |
employer |
Self-insuring employer use only — Fax or mail this page to the submitting physician/provider within 10 days of receipt or the |
authorization for treatment shall be deemed granted, per Ohio Administrative Code 4123-19-03 (K)(5). |
/ |
/ |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Self-insuring employer signature |
Date |
|
|
|
|
|
|
|
BWC-1113 (rev. 12/28/2011)
C-9 (Combines C-1-A & C-161)