Understanding the intricacies of the Pa 162 Mpg form is crucial for recipients of Medicare Assistance in Pennsylvania. This comprehensive document plays a pivotal role in the lives of individuals eligible for having their Medicare Part A and/or Part B premiums paid by the commonwealth. It offers not only a relief by covering Medicare deductibles and co-insurance but also includes essential reminders about the eligibility for Medicare Buy-In programs designed for those with limited income and resources. Additionally, the form serves as a notice to beneficiaries about increases in their Social Security checks, due to the cessation of Medicare premium deductions, and guides them on how to seek reimbursement for any premiums paid during the interim. It underscores the importance of using the ACCESS card alongside the Medicare card when accessing health care services and provides guidance on how to resolve issues or make changes to their benefits. Detailed within are instructions on how to apply for full Medical Assistance through the state’s COMPASS website or by contacting the local county assistance office (CAO). The form also lays out the appellate process for individuals dissatisfied with decisions concerning their assistance, emphasizing rights to a fair hearing and the provision of legal help. By encapsulating such critical information, the Pa 162 Mpg form acts as an essential navigational tool for beneficiaries through the complexities of Medicare assistance within Pennsylvania.
| Question | Answer |
|---|---|
| Form Name | Pa 162 Mpg Form |
| Form Length | 3 pages |
| Fillable? | No |
| Fillable fields | 0 |
| Avg. time to fill out | 45 sec |
| Other names | pa fs 162 s, pa 162vr form, pa 162, dpw |
CAO RETURN ADDRESS
|
|
www.dpw.state.pa.us |
|
|
OFFICE OF INCOME MAINTENANCE |
||
NOTICE |
COMPASS |
|
|
|
|
www.compass.state.pa.us |
|
|
|
|
|
|
Notice ID: |
|
|
|
Record Number: |
|
|
|
District: |
Case Load: |
|
|
Worker: |
|
|
|
Phone: 1- |
|
|
|
Mailing Date: |
|
|
|
Reason: |
Option: |
Type: |
|
Category: PG |
PSC: 00 |
TT: |
|
|
|
|
IMPORTANT INFORMATION ABOUT YOUR MEDICAL ASSISTANCE
The person(s) listed is/are eligible to have their Medicare Part A and/or Part B paid by the commonwealth effective mth/yr.
If you are currently enrolled in Medicare Part A and/or Part B and are paying a premium for Part A and/or Part B, your Social Security check will increase when the Medicare Part A and/or Part B premium is no longer being deducted from your check. We will also reimburse you for any premiums paid in the interim. In addition to your Medicare premium, Pennsylvania will also pay your Medicare deductibles and
You are receiving this notice because the Social Security Administration gave us information that you were interested in Pennsylvania determining your eligibility for Medicare
IfyouareinterestedinapplyingforfullMedicalAssistance,pleasecontactyourlocalCAOorapplyathttps://www.compass.state.pa.us.
If you need help applying for full Medical Assistance or have questions about this notice, you can call APPRISE at
Citation: 55 Pa. Code §§ 140.221 and 181.1
APPEAL AND FAIR HEARING
If you disagree with our decision, you have the right to appeal. See attached form for a complete explanation of your right to appeal and to a fair hearing.
If you are currently receiving benefits and your oral request for a hearing is received in the county assistance office, CAO, or your written request is postmarked or received on or before _____________________ your assistance will continue pending the hearing decision,
except when the change is due to State or Federal law.
LEGAL HELP IS AVAILABLE AT
APPLICANT NAME AND ADDRESS
CAO ADDRESS
CO |
RECORD |
DIST |
CAT |
PSC |
TT |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Notice ID:
Worker:
Phone: 1-
Mailing Date:
Reason: Option: Type:
IF YOU WISH TO APPEAL, COMPLETE THE BACK OF THIS FORM AND RETURN THE BOTTOM PORTION TO CAO.
Page 1 |
PA162 MPG 3/10 |
|
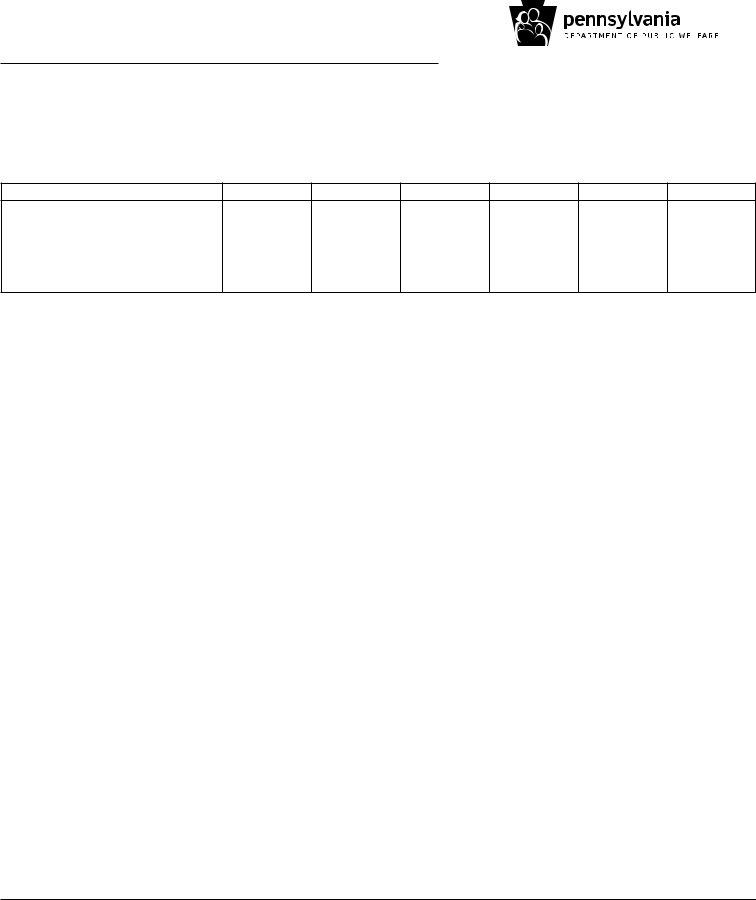
The following person(s) are affected by the action on the |
|
|||
SECTION A: |
|
||||
front of this notice. |
|
|
|||
|
|
www.dpw.state.pa.us |
|||
LINE FIRST NAME |
ACCESS/INDIVIDUAL NUMBER V |
BENEFIT PACKAGE |
|||
|
|||||
OFFICE OF INCOME MAINTENANCE
COMPASS
www.compass.state.pa.us
SECTION B: |
MA Eligibility Decision: This income covers the |
month period from |
|
|
|
The following person(s) income or financial information was included for each month for the determination of your MA benefits.
Name Income
The following calculation represents |
months of income: |
|
|
|
||||
|
|
|
|
|
|
|
|
|
Total Income |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Deductions |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Net Income |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Income Limit |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Patient Pay |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
PATIENT PAY |
|
|
|
|
|
SPEND DOWN: |
|
|
|
|
|
|
|
|
|
||
You are responsible for $ |
|
patient pay amount |
The following medical bills have been included in the |
|||||
to providers as indicated below: |
|
|
|
deductions to determine eligibility for MA Benefits for you |
||||
|
|
|
|
|
|
and your family. These unpaid bills are your responsibility |
||
|
|
|
|
|
|
and will not be paid by MA. |
|
|
Name |
Date |
Pay to: Provider |
Amount |
Name of Provider |
Date of Service |
Amount |
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
IF YOU WISH TO APPEAL, PLEASE COMPLETE AND RETURN THE BOTTOM PORTION OF THIS FORM
- - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - -
Please check the box next to the type of hearing you want:
I want a telephone hearing. I and my witnesses and anyone helping me will be at this phone number:____________________________
I want a telephone hearing. I and my witnesses and anyone helping me will be at the county assistance office, or CAO.
I want a face to face hearing. I and my witnesses and anyone helping me will be in the hearing room with the Judge and the caseworker and CAO staff.
I want a face to face hearing. I and my witnesses and anyone helping me will be in the hearing room with the judge. The caseworker and other staff will be on the phone from the CAO.
For the Hearing:
Please check if you need special help because of a hearing impairment or disability. Describe:___________________________________
Please check if you need an interpreter. There will be no cost to you. What language? ___________________________________________
I WANT TO ASK FOR A HEARING BECAUSE: (Attach more pages if you need to.)
CLIENT SIGNATURE |
ADDRESS |
TELEPHONE NO. |
DATE |
|
|
|
|
SIGNATURE CLIENT REP |
ADDRESS |
TELEPHONE NO. |
DATE |
Page 2 |
PA162 MPG 3/10 |
YOUR RIGHT TO APPEAL AND TO A FAIR HEARING
You have the right to appeal any department action or failure to act and to have a hearing if you are dissatisfied with any decision to refuse, discontinue, change, suspend, or reduce cash, medical assistance (MEDICAID), food stamps or Family Works services/benefits.
www.dpw.state.pa.us
OFFICE OF INCOME MAINTENANCE
COMPASS
www.compass.state.pa.us
However, if a change in your CASH ASSISTANCE BENEFITS, FOOD STAMPS, SOCIAL SERVICES, MEDICAL ASSISTANCE (MEDICAID) or FAMILY WORKS SERVICES/BENEFITS, is caused by State or Federal law requiring mass grant adjustment for classes of recipients, you will not be granted a hearing unless you are appealing the correctness of your grant computation, or the facts in your case.
If you are only challenging the law, your appeal will be dismissed by the Department but may be appealed to a higher court.
At the hearing you can present to the Hearing Officer the reasons why you think the decision of the County Assistance Office is incorrect and present evidence or witnesses in your own behalf.
You have the right to represent yourself or to have anyone represent you. A staff member of the County Assistance Office will refer you for free legal help upon request.
If you need an interpreter at the hearing because you do not speak English or you have limited understanding of English, or you have a hearing impairment, the Department will arrange for an official interpreter at no cost to you. You may bring a friend or relative to assist you at the hearing, but the interpreter provided by the Department will be the official interpreter. If you require any reasonable or special accommodation because of a hearing impairment (or other disability), the necessary arrangements will be made to provide the accommodation. You must make the request for an interpreter or other accommodation in advance of the hearing.
If you and your representative would like to meet with County Assistance Office staff to discuss the matter informally or to present information which might change the proposed action, please call your worker.
This will not delay or replace your fair hearing.
If the decision affects your CASH ASSISTANCE BENEFITS, SOCIAL SERVICES, MEDICAL ASSISTANCE (MEDICAID), or FAMILY WORKS SERVICES/BENEFITS, you must request a hearing within 30 days of the mailing date of this notice.
If your request is not postmarked or received within the
If this decision affects your FOOD STAMPS, you must request a hearing within 90 days from the beginning date of the change of the benefit.
If your request is not postmarked or received within the
If you are receiving CASH ASSISTANCE BENEFITS, FOOD STAMPS, SOCIAL SERVICES, MEDICAL ASSISTANCE, or FAMILY WORKS SERVICES/BENEFITS and your oral or written request for a hearing is postmarked or received within 10 days of the mailing date of this notice either your benefits will continue or your benefits will be reinstated (if there was a decrease or closing of your case because of information you gave us on a Semiannual Reporting Form) pending the outcome of the hearing. However, in those appeals where the only issue is in regard to Federal, State law or policy, your benefits will be terminated when the decision is made by the Bureau of Hearings and Appeals.
If your benefits are continued and the decision is in favor of the county assistance office, any assistance you received from the date the action would have been effective to the date the hearing order is implemented must be paid back to the Department.
If you do not want your food stamps to continue at the current amount pending the hearing decision, check () the block in the Appeal Section of the Advance Notice.
This option does not apply to the Notice to Applicant or Confirming Notice.
Federal law limits when health coverage may be denied or limited for a
Page 3 |
PA162 MPG 3/10 |