Medicare Part B Special Enrollment Period
What is a Special Enrollment Period?
Under Medicare law, a Special Enrollment Period (SEP) allows you to enroll in Medicare Part B outside of your Initial Enrollment Period (IEP) and the General Enrollment Period (GEP). If you meet the eligibility criteria and the Social Security Administration grants you an SEP, your Medicare coverage will either be effective on the first of the month that you enroll, or on the first of the following month, depending on your specific situation.* SEPs do not allow you to enroll in Medicare retroactively.
Who is eligible for a Part B SEP?
To be eligible for an SEP to enroll into Part B you must answer YES to ALL of the following three questions:
1.Are you eligible for Medicare due to age or disability? (If you are eligible due to End-Stage Renal Disease, you are not entitled to an SEP.)
2.When you first became eligible for Medicare, were you enrolled in either Medicare Part B or an employer group health plan based on your current employment or the current employment of a spouse or other family** member? (If you did not have any health coverage or you had only retiree coverage or COBRA when you first became eligible for Medicare, you are not entitled to an SEP.)
3.Have you been continuously covered either by Medicare Part B or by a group health plan based on your current employment or the current employment of a spouse or other family** member from the
time you became eligible for Medicare until now, with no more than eight consecutive months of lapses in coverage? (A “lapse” in coverage is defined as a period of time when you have neither
Medicare Part B nor group health coverage based on current employment. For example, if you only had COBRA or retiree coverage at any time since you became eligible for Medicare, this is considered a lapse in coverage. If your lapse in coverage exceeded eight consecutive months, then you are not eligible for an SEP.)
If you answered YES to all three questions above, then you are usually eligible for an SEP.
If you answered NO to any of the above questions, you are not eligible for an SEP and may have to wait for the next General Enrollment Period to enroll in Medicare Part B. There may be other ways you can enroll in Medicare Part B outside of an enrollment period, for example, if you qualify for Equitable Relief or a Medicare Savings Program.
© 2012 Medicare Rights Center |
Helpline: 800-333-4114 |
www.medicareinteractive.org |

How can I obtain a Part B SEP?
To obtain an SEP to enroll into Part B, contact the Social Security Administration (SSA) at
800-772-1213 and request the following two forms:
 CMS 40B (Application for Enrollment in Medicare)
CMS 40B (Application for Enrollment in Medicare)
CMS L564 (Request for Employment Information)
Fill out and sign form CMS 40B and have your employer (or your spouse or family member’s employer) fill out form CMS L564. Once complete, bring both forms with an accompanying cover letter to your local Social Security office. (See the attached Part B SEP cover letter for assistance.)
If you, your spouse or family member** have had coverage based on current employment from multiple employers since you became eligible for Medicare, then you should request several copies of form CMS L564 and ask each employer to fill it out.
The purpose of this form is to provide documentation to Social Security that proves that you’ve been continuously covered by a group health plan based on current employment, with no more than eight consecutive months of lapses in coverage.
There may be times when your former employer will be unable to fill out this form. For example, an employer may have gone out of business or may not have adequate records. If you are not able to get previous employers to fill out form L564, contact the Medicare Rights Center for information on how to obtain alternative documents to prove continuous coverage.
Once your have obtained all the needed documents, be sure to make copies of everything you submit to SSA. When submitting your documents, get a receipt from an SSA office representative indicating the date you submitted the documents.
You will receive a letter in the mail from SSA either approving or denying your enrollment. If you are denied enrollment, you will have the right to appeal this decision.
*If you request an SEP while you are covered by a group health plan based on current employment or within a month after you lose your group health plan based on current employment, you can delay your Part B start date for up to three months.
**If you qualify for Medicare based on disability and you have a group health plan from a family member other than your spouse, you are only eligible for an SEP if there are 100 or more people employed by the company. If the company employs fewer than 100 people, family members other than spouses are not eligible for the SEP.
© 2012 Medicare Rights Center |
Helpline: 800-333-4114 |
www.medicareinteractive.org |
Sample Letter to SSA for Medicare Part B
Special Enrollment Period
[Date]
Social Security Administration
[Address of local office]
Re: Medicare Part B Special Enrollment Period
Beneficiary: [Name]
SSN: [Social Security Number]
To whom it may concern,
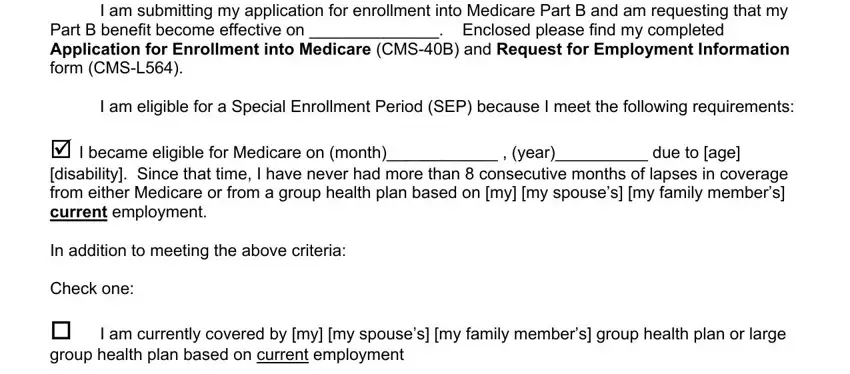
I am submitting my application for enrollment into Medicare Part B and am requesting that my Part B benefit become effective on ______________. Enclosed please find my completed
Application for Enrollment into Medicare (CMS-40B) and Request for Employment Information form (CMS-L564).
I am eligible for a Special Enrollment Period (SEP) because I meet the following requirements:
I became eligible for Medicare on (month)____________ , (year)__________ due to [age]
[disability]. Since that time, I have never had more than 8 consecutive months of lapses in coverage from either Medicare or from a group health plan based on [my] [my spouse’s] [my family member’s]
current employment.
In addition to meeting the above criteria:
Check one:
I am currently covered by [my] [my spouse’s] [my family member’s] group health plan or large group health plan based on current employment
OR
I am not currently covered by a group health plan or large group health plan based on current employment at this time. However, I was covered by [my] [my spouse’s] [my family member’s] employer group health plan based on current employment within the last 8 months. I lost my employer group plan based on current employment on (month)____________
(year)_____________.
© 2012 Medicare Rights Center |
Helpline: 800-333-4114 |
www.medicareinteractive.org |

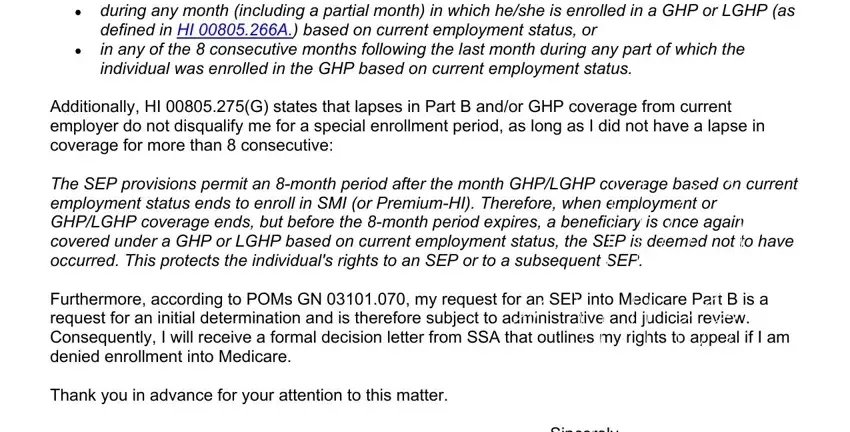
According to Social Security’s Program Operations Manual section HI 00805.275 SEP Enrollments:
Beginning 3/95, individuals who are age 65 and over or disabled, can enroll (or reenroll) in SMI and/or Premium-HI:
during any month (including a partial month) in which he/she is enrolled in a GHP or LGHP (as defined in HI 00805.266A.) based on current employment status, or
in any of the 8 consecutive months following the last month during any part of which the individual was enrolled in the GHP based on current employment status.
Additionally, HI 00805.275(G) states that lapses in Part B and/or GHP coverage from current employer do not disqualify me for a special enrollment period, as long as I did not have a lapse in coverage for more than 8 consecutive:
The SEP provisions permit an 8-month period after the month GHP/LGHP coverage based on current employment status ends to enroll in SMI (or Premium-HI). Therefore, when employment or GHP/LGHP coverage ends, but before the 8-month period expires, a beneficiary is once again covered under a GHP or LGHP based on current employment status, the SEP is deemed not to have occurred. This protects the individual's rights to an SEP or to a subsequent SEP.
Furthermore, according to POMs GN 03101.070, my request for an SEP into Medicare Part B is a request for an initial determination and is therefore subject to administrative and judicial review. Consequently, I will receive a formal decision letter from SSA that outlines my rights to appeal if I am denied enrollment into Medicare.
Thank you in advance for your attention to this matter.
Sincerely,
[Your name]
[Your title]
Attachments: [list any attachments]
© 2012 Medicare Rights Center |
Helpline: 800-333-4114 |
www.medicareinteractive.org |


 CMS 40B (Application for Enrollment in Medicare)
CMS 40B (Application for Enrollment in Medicare)
