We were establishing our PDF editor having the notion of making it as easy to work with as possible. This is why the process of filling out the Meningococcal will be smooth follow these steps:
Step 1: Initially, hit the orange button "Get Form Now".
Step 2: At the moment you are on the form editing page. You can enhance and add text to the document, highlight words and phrases, cross or check particular words, insert images, put a signature on it, get rid of unnecessary fields, or eliminate them altogether.
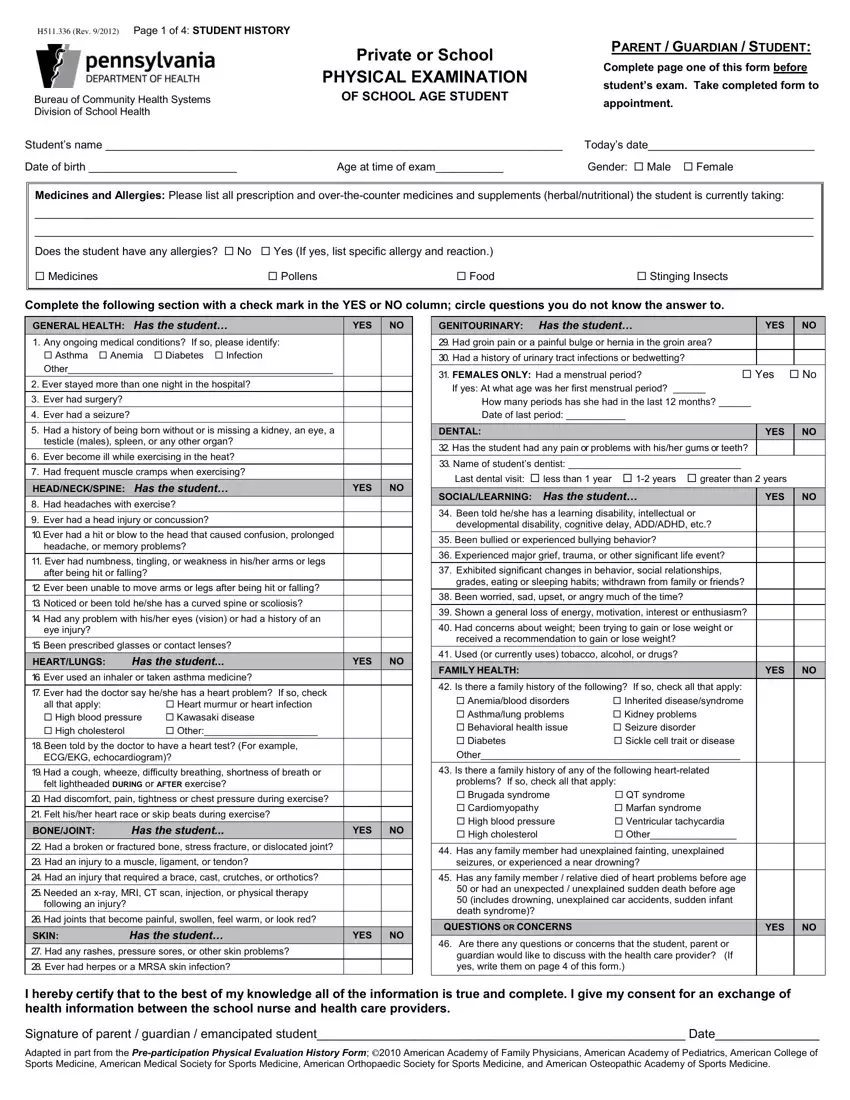
Get the Men, in, go, co, c, cal PDF and provide the material for each part:
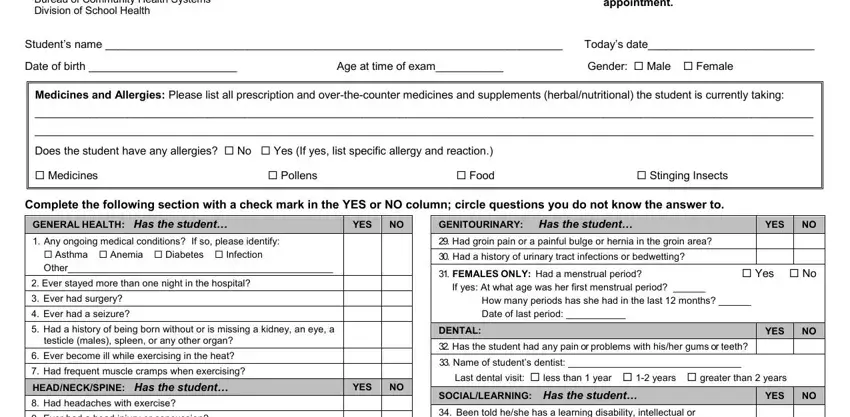
The application will expect you to complete the Ever, had, ahead, injury, or, concussion headache, or, memory, problems after, being, hit, or, falling eye, injury HEART, LUNGS, Has, the, student YES, NO ECG, EKG, echo, cardiogram BONE, JOINT, Has, the, student YES, NO following, an, injury Ever, had, herpes, or, a, MRSA, skin, infection YES, NO FAMILY, HEALTH YES, NO and problems, If, so, check, all, that, apply box.
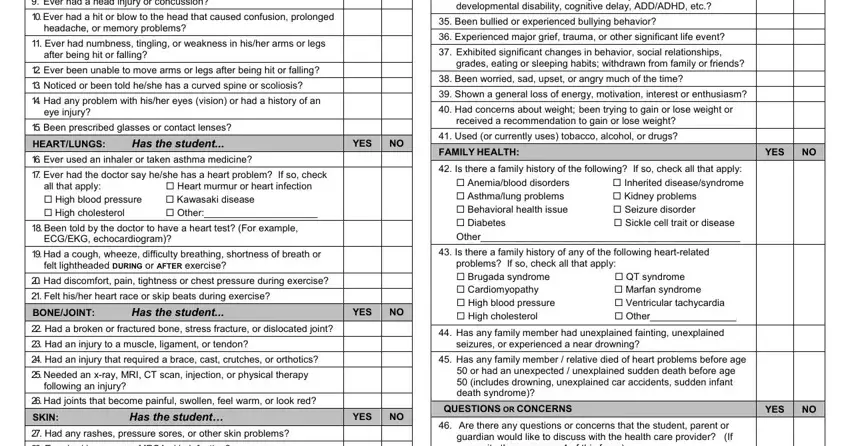
The program will require details to easily fill in the box .
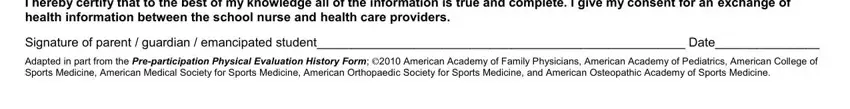
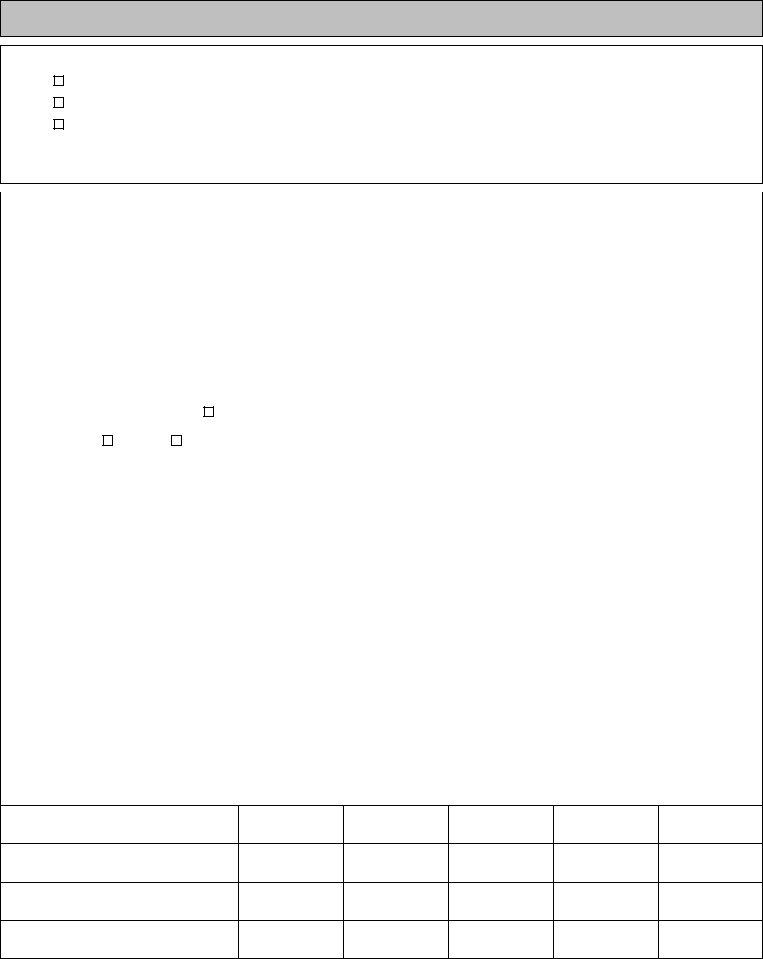
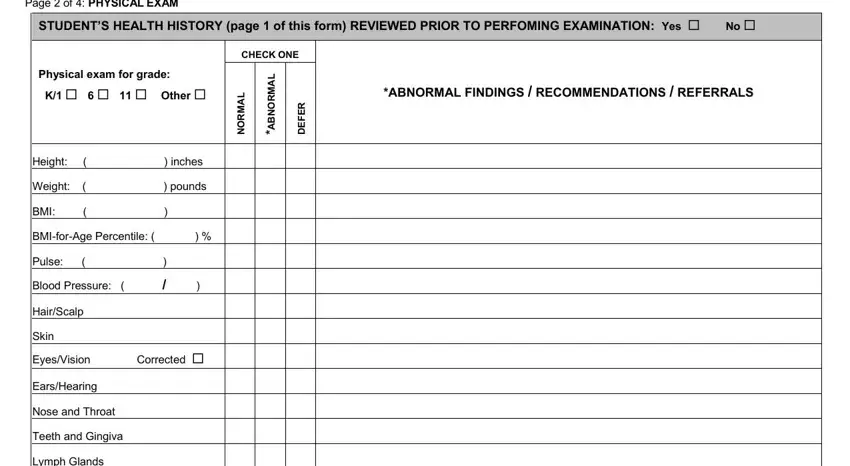
The Page, of, PHYSICAL, EXAM CHECK, ONE L, AMRO, NBA LA, MR, ON RE, FED Height, inches Weight, pounds BMI, BMI, forAge, Percentile Pulse, Blood, Pressure Hair, Scalp Skin, Eyes, Vision, Corrected and Ears, Hearing area has to be used to provide the rights or obligations of each party.
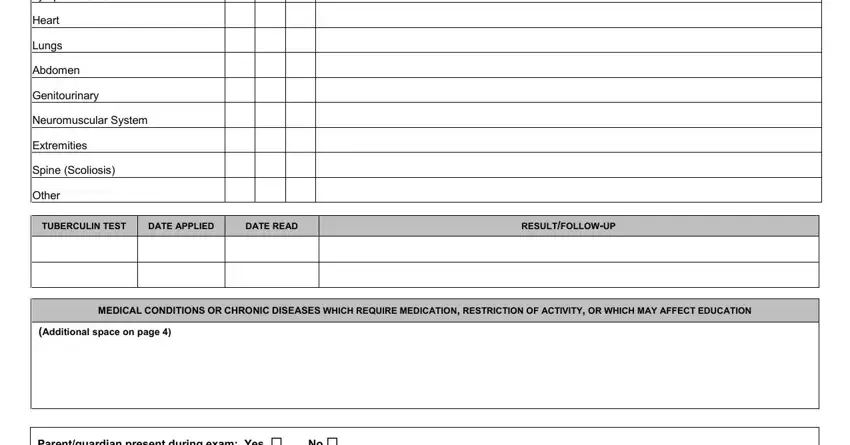
Finalize by reviewing the next fields and preparing them as needed: Lymph, Glands Heart, Lungs, Abdomen, Genitourinary, Neuromuscular, System Extremities, Spine, Scoliosis Other, TUBER, CUL, IN, TEST DATE, APPLIED DATE, READ RESULT, FOLLOWUP and Additional, space, on, page
Step 3: After you choose the Done button, your finished file can be exported to any of your devices or to email given by you.
Step 4: You should make as many copies of the file as possible to remain away from potential worries.