banner health authorization form can be completed in no time. Simply try FormsPal PDF tool to complete the job promptly. FormsPal professional team is relentlessly working to enhance the editor and ensure it is much better for users with its multiple functions. Uncover an constantly progressive experience now - check out and uncover new opportunities along the way! Getting underway is simple! All you should do is take these basic steps down below:
Step 1: Open the PDF file inside our editor by clicking on the "Get Form Button" at the top of this webpage.
Step 2: With the help of this handy PDF editor, it is easy to do more than just fill in blank form fields. Edit away and make your docs look faultless with custom text incorporated, or adjust the original content to excellence - all that backed up by an ability to insert stunning images and sign the file off.
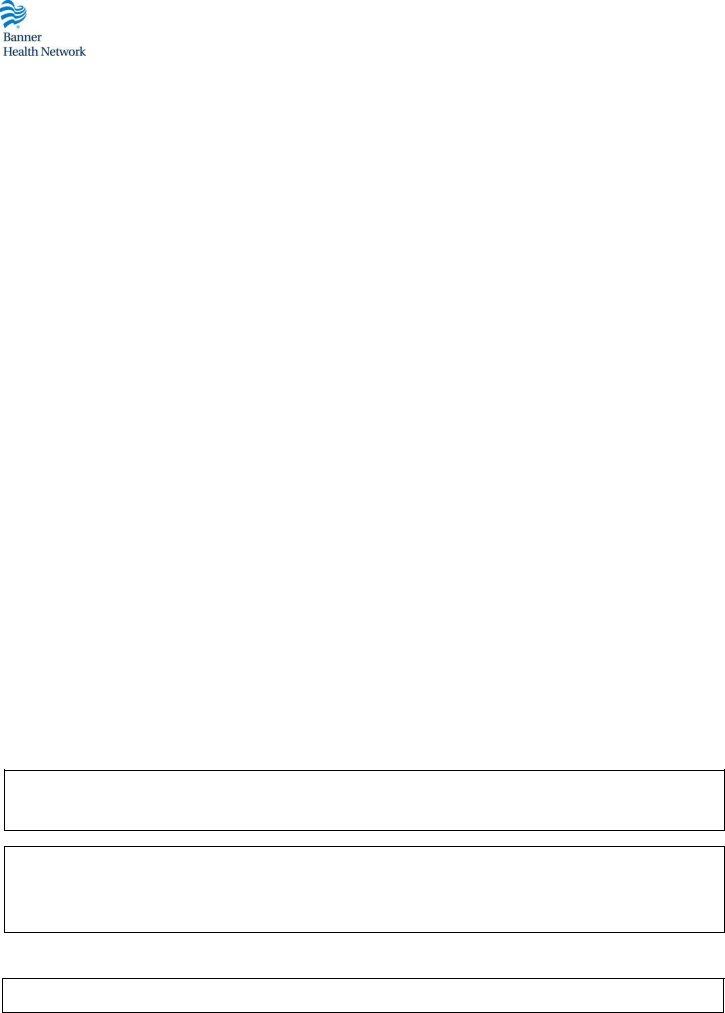
With regards to the blanks of this particular document, here's what you need to do:
1. While completing the banner health authorization form, make certain to complete all important blank fields in their corresponding area. This will help to expedite the work, allowing your information to be processed swiftly and accurately.
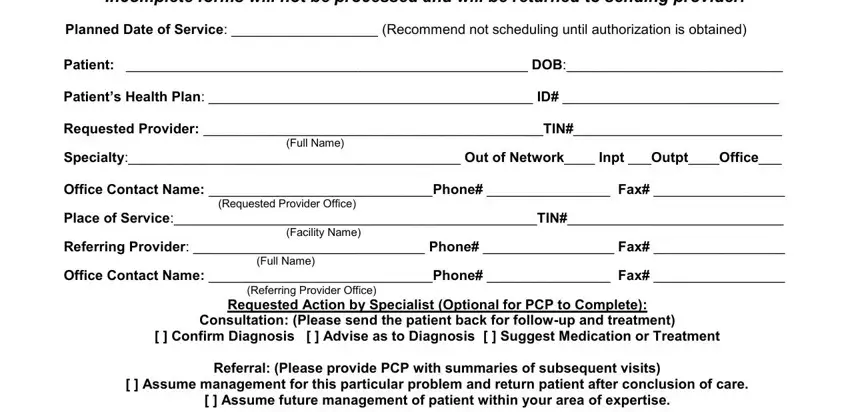
2. After this segment is finished, it's time to put in the needed particulars in DiagnosisICD TreatmentProcedure, THE FOLLOWING APPLIES ONLY TO, To access your Banner Option, and For Banner Use Only allowing you to move forward further.
It is possible to get it wrong while filling in the THE FOLLOWING APPLIES ONLY TO, therefore ensure that you reread it prior to when you finalize the form.
Step 3: Just after proofreading the fields you've filled in, click "Done" and you are done and dusted! Acquire your banner health authorization form the instant you subscribe to a free trial. Readily view the pdf form within your FormsPal account, with any edits and changes all synced! At FormsPal.com, we do our utmost to make sure that all of your information is maintained protected.