S.T.A.B.L.E. Pre-Assessment
1
S.T.A.B.L.E. Program Pre-Assessment
Please write your name and answers on the answer sheet. For the following multiple-choice questions, choose the one best answer.
1.The following are appropriate methods for rewarming a hypothermic infant:
1)Cover with plastic from chin to feet. Fill latex gloves with hot water and place along both sides of infant’s body
2)Place in incubator and increase environmental air temperature
3)Place infant on top of an activated chemical thermal mattress, after the mattress is covered with a thin cloth
4)Place on radiant warmer on servo-control mode
5)Heat a blanket in a microwave for 15 seconds, then place blanket around infant
a)1, 2, 3
b)2, 3, 4
c)3, 4, 5
2.A 40-week gestation infant born by cesarean section for cephalopelvic disproportion was well until 18 hours of life when he developed respiratory distress, characterized by tachypnea, grunting, retracting, nasal flaring, and cyanosis. 100% oxygen was provided by face mask however oxygen saturation failed to rise above 85%. The infant required endotracheal intubation and ventilation. Given this limited history, which of the following diagnoses are most likely?
a)Bacterial sepsis, Pneumonia, Persistent Pulmonary Hypertension of the Newborn (PPHN)
b)Viral sepsis, Respiratory Distress Syndrome, Cyanotic congenital heart disease
c)Septicemia, Transient Tachypnea of the Newborn (TTNB), Coarctation of the Aorta
3.Hypoglycemia may result in an infant of a diabetic mother because of:
a)The mother’s elevated glucose levels during pregnancy
b)The mother’s use of insulin during pregnancy
c)The mother’s elevated cortisol levels during pregnancy
S.T.A.B.L.E. Pre-Assessment
2
4.Bacterial sepsis is suspected in a one-day old infant with severe hypotension. Two 10 ml/kg boluses of normal saline are given, however the pulses are still weak, capillary refill time is prolonged, and the infant remains hypotensive. Dopamine is ordered. Which one of the following physician orders is correct?
a)Give a loading dose of dopamine, 5 micrograms per kilogram, followed by a continuous infusion of dopamine 10 micrograms per kilogram per minute IV.
b)Give dopamine 5 micrograms per kilogram per minute via the peripheral IV or umbilical vein.
c)Give dopamine 5 micrograms per kilogram per minute via the umbilical vein or artery.
5.Pre and post-ductal saturation monitoring is ordered for an infant with suspected persistent pulmonary hypertension. Where will the two oximeter probes be placed AND what will each probe be measuring?
a)Left hand (pre-ductal saturation), Right foot (post-ductal saturation)
b)Left hand (post-ductal saturation), Right foot (pre-ductal saturation),
c)Right hand (pre-ductal saturation), Left foot (post-ductal saturation)
6.The function of brown fat is to:
a)Generate heat when it is metabolized
b)Provide a rapidly available source of glucose in the first day of life
c)Provide an insulating layer of fat in the first month of life
7.A term infant develops severe respiratory distress following aspiration of stomach contents. Following endotracheal intubation, the infant is given positive pressure ventilation with 100% oxygen. The oxygen saturation does not rise above 65%. What problems might occur in this infant?
1)Pulmonary vascular resistance may increase and cause right-to-left shunting at the ductus arteriosus
2)Tissue hypoxia may lead to cell and organ damage
3)Increased glucose utilization may result in hypoglycemia
4)Development of metabolic acidosis following conversion to anaerobic metabolism
a)1 and 3 are correct
b)2 and 4 are correct
c)All are correct
S.T.A.B.L.E. Pre-Assessment
3
8.A mother is concerned because her six-hour old infant is overly sleepy and she thinks there is an increase in bruising of the scalp. Inspection of the delivery record reveals shoulder dystocia with forceps assisted delivery which was reportedly ‘difficult’. Apgars were 7 at one minute and 8 at
five minutes. In the nursery, the vital signs and exam are: Axillary temperature 36.2 C (97.2 F)
Respiratory rate 80 per minute Mild intercostal retractions Oxygen saturation 85% Capillary refill time 5 seconds Brachial and femoral pulses are weak Hypotonic muscle tone, weak cry
Head circumference 36 centimeters (34 centimeters at birth)
Scalp palpation reveals swelling that extends across suture lines from the front of the anterior fontanelle to the ears on both sides and back to the posterior fontanelle
Given this limited information, which of the following should be strongly suspected?
a)Caput succedaneum
b)Cephalohematoma
c)Subgaleal hemorrhage
9.Endotracheal intubation with positive pressure ventilation should be performed without delay if:
1)You are unable to ventilate and/or oxygenate adequately with bag/mask ventilation
2)The infant is gasping
3)The infant is being transported to another facility
4)The infant has a pneumothorax
a)1, 2
b)3, 4
c)All are correct
S.T.A.B.L.E. Pre-Assessment
4
Matching.
Infants with the following conditions or physical findings are at risk to develop hypoglycemia. Match the reason for becoming hypoglycemic from the “Causes” column on the right side (choose only one answer per question).
CAUSES
10. |
Infant of a diabetic mother |
a |
b |
c |
11. |
Term, small for gestational |
a |
b |
c |
|
age infant |
|
|
|
12. |
Term newborn in cardiogenic |
a |
b |
c |
|
shock |
|
|
|
13. |
Large for gestational age |
a |
b |
c |
14. |
Premature infant |
a |
b |
c |
a)Decreased glycogen stores
b)Hyperinsulinism
c)Increased utilization of glucose and glycogen stores
15.An infant is breathing 80 times per minute. An arterial blood gas reveals a pH of 7.20 and a PCO2 of 25. Which one of the following conditions should be suspected?
a)Congenital heart disease such as coarctation of the aorta or aortic atresia
b)Pneumonia
c)Congenital diaphragmatic hernia
16.An infant is cyanotic at rest but ‘pinks up’ with crying. You suspect the infant may have:
a)Cyanotic congenital heart disease
b)Transient tachypnea of the newborn
c)Choanal atresia
17.A neonate is experiencing severe respiratory distress in the delivery room. When bag/mask ventilation and oxygen are provided, the infant deteriorates further. The abdomen appears sunken. Which action should be strongly considered?
a)Place in hood oxygen and achieve an oxygen saturation greater than 90%
b)Initiate continuous positive airway pressure with 6 to 8 cm H20 pressure
c)Perform endotracheal intubation and assist ventilation
S.T.A.B.L.E. Pre-Assessment
5
18.Cardiogenic shock may result because of:
a)Subgaleal hemorrhage, placental abruption, arrhythmias
b)Hypoxia, bacterial infection, severe hypoglycemia
c)Intraventricular hemorrhage, tension pneumothorax, viral infection
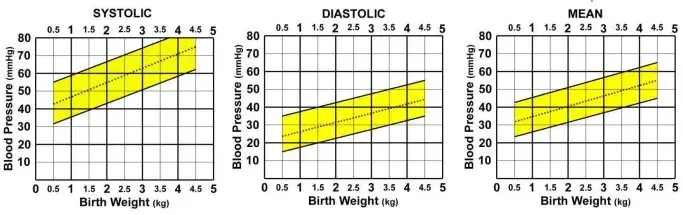
19.8-hour old, 38-week gestation, 3.2 kilogram infant with a blood pressure of 45/23 (mean 34). Plot the BP on the graph and determine if the blood pressure is:
a)Low
b)Low-normal
c)Normal
(Shaded area between the solid diagonal lines is considered normal)
20.At one hour of life, a term infant weighing 1400 grams (3 pounds, 1.5 ounces) has a serum glucose of 10 mg/dL (0.55 mmol/L). Which of the following orders is the most appropriate therapy in this situation:
a)Begin an intravenous (IV) infusion of D10W at 5 mls per hour (80 mls per kilogram per day). Recheck the blood glucose in one hour.
b)Give 2.8 mls D10W IV slow push, then begin an IV infusion of D10W at 5 mls per hour (80 mls per kilogram per day).
c)Confirm the blood glucose by sending another sample to the lab. If low, give 4 mls/kg D25W IV slow push followed by an IV infusion of D10W at 5 mls per hour (80 mls per kilogram per day).
21.The normal response to cold stress in term infants includes which of the following?
1)Vasodilatation of the coronary arteries
2)Brown fat metabolism
3)Pulmonary vasoconstriction
4)Peripheral vasoconstriction
5)Decreased oxygen consumption
6)Decreased muscle activity and flexion
a)1, 2, 4, 5
b)2, 3, 4
c)All are correct
Edition 7
S.T.A.B.L.E. Pre-Assessment
6
22.A 39-week gestation infant delivered at home is unresponsive and requires mouth-to-mouth resuscitation. The infant is transported to the emergency room where you are asked to assist with resuscitation. When you arrive, the infant is lying undressed on the examination table, intubated, and being hand-ventilated with 100% oxygen at a rate of 40 breaths per minute. There are no spontaneous respirations or movement, the pulses are weak, and capillary refill time is 5 seconds. There is no intravenous line in place. The vital signs at this point are:
Temperature 34 degrees Celsius (93.2 degrees Fahrenheit) Heart rate 100 beats per minute
Respiratory rate 40 (by assisted ventilation) A blood pressure has not been obtained
Which of the following stabilization options should be performed immediately?
1)Establish intravenous access by placing a peripheral intravenous line and administer a 2 ml/kilogram bolus of D25W
2)Move the infant to a radiant warmer, assess patency of the airway, confirm the endotracheal tube is in correct position and well secured
3)Establish intravenous access by placing an umbilical venous catheter and administer a 10 ml/kilogram bolus of normal saline
a)1 and 2
b)2 only
c)2 and 3
The following blood gases are from arterial sites.
23.pH 7.25, PCO2 36, HCO3 (bicarbonate) 15. The correct interpretation of this blood gas is:
a)Uncompensated metabolic acidosis
b)Compensated respiratory acidosis
c)Uncompensated mixed metabolic and respiratory acidosis
24.pH 7.15, PCO2 63, HCO3 (bicarbonate) 21. The correct interpretation of this blood gas is:
a)Uncompensated metabolic acidosis
b)Uncompensated respiratory acidosis
c)Uncompensated mixed metabolic and respiratory acidosis
25.pH 7.0, PCO2 55, HCO3 (bicarbonate) 14. The correct interpretation of this blood gas is:
a)Uncompensated metabolic acidosis
b)Uncompensated respiratory acidosis
c)Uncompensated mixed metabolic and respiratory acidosis
S.T.A.B.L.E. Pre-Assessment
7
26.pH 7.35, PCO2 23, HCO3 (bicarbonate) 12. The correct interpretation of this blood gas is:
a)Compensated metabolic acidosis
b)Compensated respiratory acidosis
c)Compensated mixed metabolic and respiratory acidosis
27.Which organ is most likely to be adversely affected by severe, persistent hypoglycemia?
a)Liver
b)Kidney
c)Brain
28.A neonate with a pneumothorax may exhibit which of the following symptoms:
1)Increased work of breathing
2)Bradycardia
3)Asymmetric appearing chest
4)Cyanosis
5)Decreased femoral pulses
a)1, 3, 5
b)1, 2, 4
c)All are correct
29.A 3-kilogram infant requires intubation for severe respiratory distress. The endotracheal tube is taped at 9 centimeters at the lip. The endotracheal tube tip is most likely:
a)Too high
b)In good position
c)Too low
30.An infant is born at 42 weeks gestation. Apgars are 3 at one minute, and 5 at five minutes. At 10 minutes of life, the heart rate drops to 60 beats per minute and gasping respirations are noted. The infant is intubated, given assisted ventilation with oxygen, and chest compressions are started. This infant is at risk to develop what complications?
1)Hypoglycemia
2)Acidosis
3)Pneumothorax
4)Seizures
5)Retinal damage from oxygen exposure
a)2 and 3
b)1, 2, 3, 4
c)All are correct
S.T.A.B.L.E. Pre-Assessment
8
31.An infant is breast feeding when his mother asks you to come and assess him for ‘green’ spit. You notice a lime green colored vomit. The infant’s abdomen is not distended however she appears very irritable and is crying. This history is most consistent with which diagnosis?
a)Malrotation with midgut volvulus
b)Necrotizing enterocolitis
c)Pyloric stenosis
32.An 18-hour old, 36-week gestation infant appears lethargic, develops abdominal distension and respiratory distress. A complete blood count and blood culture are obtained and antibiotics are started. The absolute neutrophil count (ANC) on three consecutive complete blood counts (CBCs) obtained eight hours apart are: 3240, 1050, and 540. Your interpretation of this trend:
a)Worrisome - because it indicates decreased inflammatory response
b)Worrisome – because it indicates possible neutrophil depletion
c)Worrisome – because it indicates both viral and bacterial infection are likely
33.The immature-to-total ratio (I/T ratio) on the same three CBCs obtained 8 hours apart are: 0.36, 0.56, and 0.83. This trend is:
a)Worrisome – because the numbers indicate an increasing proportion of total mature neutrophils
b)Worrisome – because the numbers indicate an increasing immature and total lymphocyte count
c)Worrisome – because the numbers indicate an increasing proportion of immature neutrophils
34.A 34-week gestation infant has a rectal temperature of 31 degrees Celsius (87.8 degrees Fahrenheit). Which of the following signs might be observed with this body temperature?
a)Hypertension, atrial arrhythmia, prolonged capillary refill time
b)Irritability, tachycardia, tachypnea
c)Hypotension, bradycardia, slow respirations
35.An infant delivers unexpectedly at home. When the emergency medical personnel arrive, they note the following about the infant’s appearance: very small chin and jaw, obstruction of the airway by the tongue, and extreme respiratory distress. These findings are consistent with:
a)Pierre Robin sequence
b)Tracheoesophageal fistula
c)Choanal atresia
S.T.A.B.L.E. Pre-Assessment
9
36.A 38-week gestation infant is delivered vaginally after a difficult labor. Membranes were ruptured for 20 hours and the fluid was clear. She did well initially but six hours after birth she appeared hypotonic, mottled, and required oxygen to maintain oxygen saturation greater than 90%. Symptoms included tachypnea, nasal flaring, grunting, and retractions. You are most concerned that this infant has:
a)Cyanotic congenital heart disease (cyanotic CHD)
b)Respiratory Distress Syndrome (RDS)
c)Bacterial sepsis
37.Dopamine is a drug prescribed to treat hypotension and may be administered via:
1)Peripheral vein or umbilical venous catheter (UVC)
2)Umbilical artery catheter (UAC)
3)Endotracheal tube
a)1
b)1, 2
c)All are correct
38.A 4-hour old infant is tachypneic and hypotonic. The infant’s temperature is 38.4 degrees Celsius
(101.2 degrees Fahrenheit). A complete blood count (CBC) is ordered with the following results:
WBC ………………………. 9,200
Hemoglobin ……………….. 15
Hematocrit ………………… 46
Platelets …………………… 290,000
Lymphocytes ……………… 51%
Segmented neutrophils ……. 44 %
Band neutrophils ………….. 5 %
You discuss the patient and CBC results with the infant’s healthcare practitioner who responds by saying: “The CBC is normal which reassures me that the baby is fine. I don’t think we need to do anything more than keep a close eye on the baby.”
Your assessment of this response is:
a)You agree with the healthcare practitioner because a normal CBC means this infant is very unlikely to have an infection
b)You disagree with the healthcare practitioner because a normal CBC may be observed when an infant is infected
c)You mostly agree with the healthcare practitioner except you think a CBC should be re-evaluated in six to eight hours
S.T.A.B.L.E. Pre-Assessment
10
39.Which statement(s) about hypothermia are true?
1)Hypothermia stimulates norepinephrine release, which increases metabolic rate and brown fat metabolism
2)Hypothermia causes peripheral vasoconstriction and may lead to tissue hypoxia, dependence on anaerobic metabolism, and impaired brown fat metabolism
3)Hypothermia causes pulmonary vasoconstriction which may result in right-to-left shunting through the ductus arteriosus
a)1 only
b)1 and 2
c)All are correct
40.The parents of a transported infant ask you to explain persistent pulmonary hypertension. The best explanation about this condition is:
a)The lung blood vessels are constricted which makes blood flow under pressure into the lungs. This causes fluid to leak outside of the blood vessels, which floods the lungs and interferes with the normal process of oxygenation.
b)This is a special kind of hypertension that affects the blood vessels in the lungs. It presents at birth in term and near term infants. At approximately two weeks of age, the blood pressure in the lungs will decrease and the problem will resolve. If however, the blood pressure does not decrease, a medication called Nitric Oxide can be given to treat the hypertension.
c)The lung blood vessels are constricted which prevents adequate amounts of blood from entering the lungs. Blood that normally goes to the lungs to become oxygenated is being shunted through a blood vessel called the ductus arteriosus. This causes problems with oxygenation of the blood.