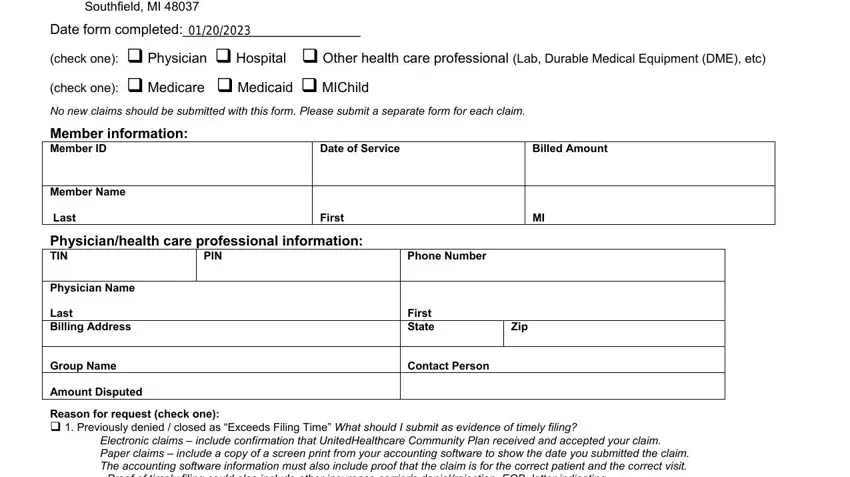
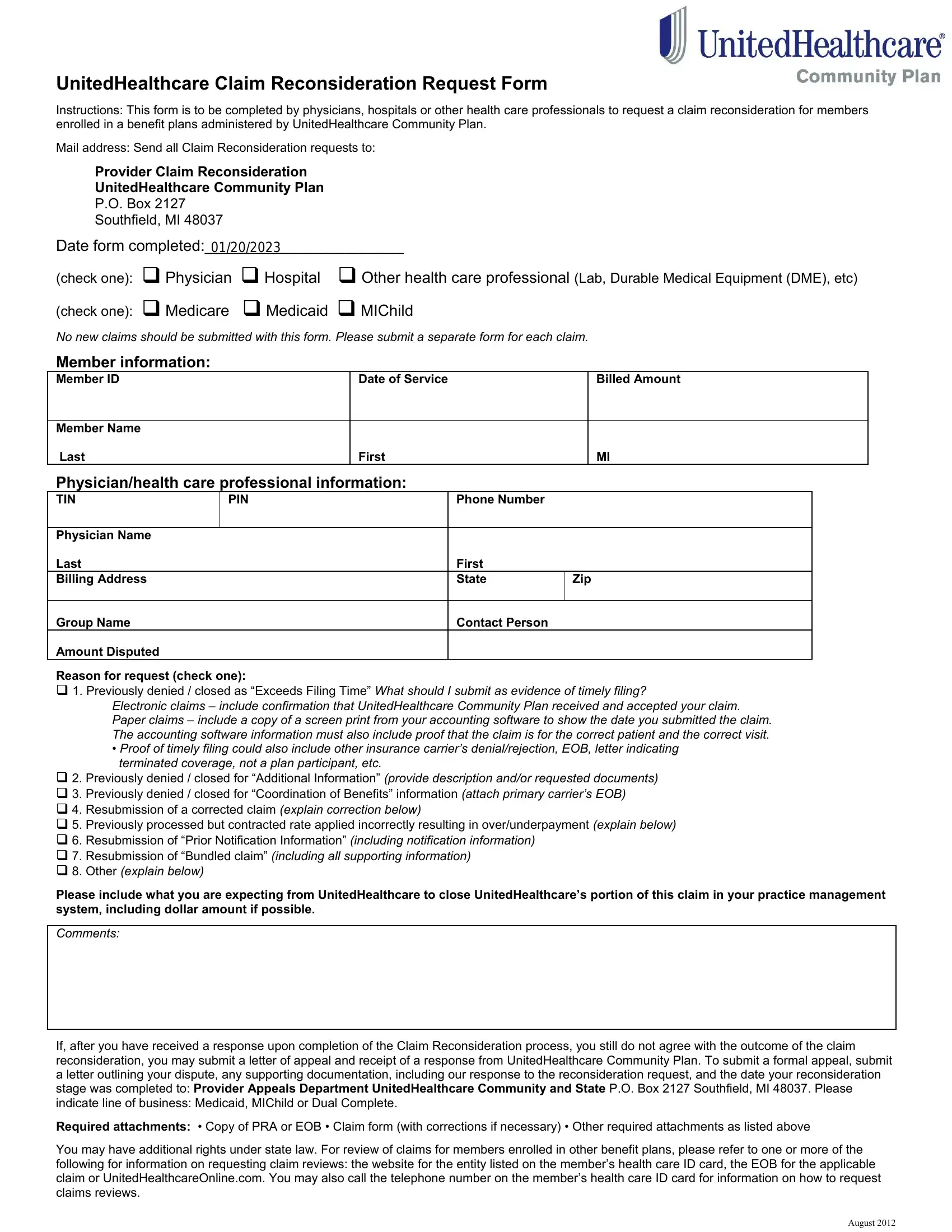
UnitedHealthcare Claim Reconsideration Request Form
Instructions: This form is to be completed by physicians, hospitals or other health care professionals to request a claim reconsideration for members enrolled in a benefit plans administered by UnitedHealthcare Community Plan.
Mail address: Send all Claim Reconsideration requests to:
Provider Claim Reconsideration
UnitedHealthcare Community Plan
P.O. Box 2127
Southfield, MI 48037
Date form completed:_______________________
(check one): Physician Hospital Other health care professional (Lab, Durable Medical Equipment (DME), etc)
(check one): Medicare Medicaid MIChild
No new claims should be submitted with this form. Please submit a separate form for each claim.
Member information:
Member ID |
|
Date of Service |
|
|
Billed Amount |
|
|
|
|
|
|
|
Member Name |
|
|
|
|
|
|
Last |
|
First |
|
|
MI |
Physician/health care professional information: |
|
|
|
|
TIN |
PIN |
Phone Number |
|
|
|
|
|
|
|
|
|
|
Physician Name |
|
|
|
|
|
|
Last |
|
|
First |
|
|
|
Billing Address |
|
|
State |
Zip |
|
|
|
|
|
|
|
|
Group Name |
|
|
Contact Person |
|
|
|
Amount Disputed |
|
|
|
|
|
|
Reason for request (check one):
1. Previously denied / closed as “Exceeds Filing Time” What should I submit as evidence of timely filing?
Electronic claims – include confirmation that UnitedHealthcare Community Plan received and accepted your claim. Paper claims – include a copy of a screen print from your accounting software to show the date you submitted the claim. The accounting software information must also include proof that the claim is for the correct patient and the correct visit.
•Proof of timely filing could also include other insurance carrier’s denial/rejection, EOB, letter indicating terminated coverage, not a plan participant, etc.
2. Previously denied / closed for “Additional Information” (provide description and/or requested documents)
3. Previously denied / closed for “Coordination of Benefits” information (attach primary carrier’s EOB)
4. Resubmission of a corrected claim (explain correction below)
5. Previously processed but contracted rate applied incorrectly resulting in over/underpayment (explain below)
6. Resubmission of “Prior Notification Information” (including notification information)
7. Resubmission of “Bundled claim” (including all supporting information)
8. Other (explain below)
Please include what you are expecting from UnitedHealthcare to close UnitedHealthcare’s portion of this claim in your practice management system, including dollar amount if possible.
Comments:
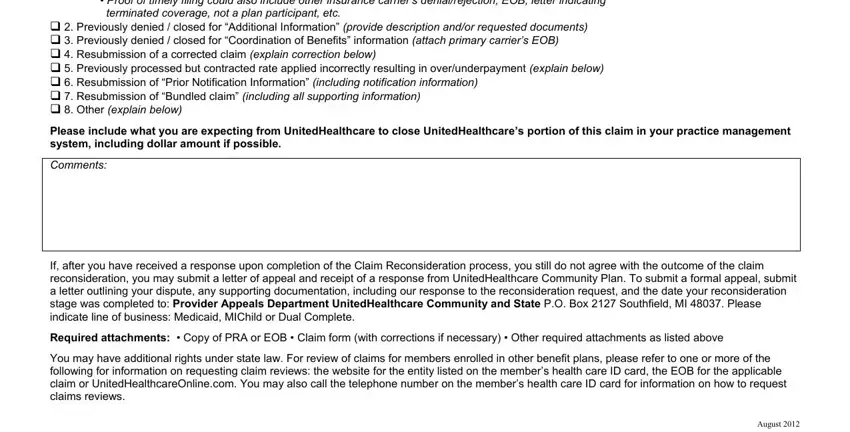
If, after you have received a response upon completion of the Claim Reconsideration process, you still do not agree with the outcome of the claim reconsideration, you may submit a letter of appeal and receipt of a response from UnitedHealthcare Community Plan. To submit a formal appeal, submit a letter outlining your dispute, any supporting documentation, including our response to the reconsideration request, and the date your reconsideration stage was completed to: Provider Appeals Department UnitedHealthcare Community and State P.O. Box 2127 Southfield, MI 48037. Please indicate line of business: Medicaid, MIChild or Dual Complete.
Required attachments: • Copy of PRA or EOB • Claim form (with corrections if necessary) • Other required attachments as listed above
You may have additional rights under state law. For review of claims for members enrolled in other benefit plans, please refer to one or more of the following for information on requesting claim reviews: the website for the entity listed on the member’s health care ID card, the EOB for the applicable claim or UnitedHealthcareOnline.com. You may also call the telephone number on the member’s health care ID card for information on how to request claims reviews.
August 2012
Claim Reconsideration Request Form
A revised UnitedHealthcare Community Plan Claim Reconsideration Request Form is now available for immediate use by physicians, hospitals and other health care professionals when requesting a claim reconsideration for members enrolled in benefit plans administered by UnitedHealthcare Community and State.
Please note that no new claims should be submitted with this form.
Health care professionals should submit a separate form for each claim.
Claim Reconsideration Request - This request will be handled as a Claim Reconsideration. This process involves a review to determine whether a claim was paid correctly, including identifying system set-up, contract load and other factors that may have resulted in the original claim being denied or reduced.
Please note that, this form should only be used for Claim Reconsiderations. A Claim Reconsideration is the first step of the Dispute Resolution Process.
Mail address: Send all Claim Reconsideration requests to:
Provider Claim Reconsideration
UnitedHealthcare Community Plan
P.O. Box 2127
Southfield, MI 48037
Once you have received a response after completion of the Claim Reconsideration process, if you still do not agree with the outcome of the claim reconsideration, you may submit a letter of appeal and receipt of a response from UnitedHealthcare Community and State. To submit a Formal Appeal, you should submit a letter outlining your dispute, any supporting documentation, including our response to the reconsideration request, and the date your reconsideration stage was completed to:
Mail all UnitedHealthcare Community Plan Medicaid/MIChild Provider Appeal requests to:
Provider Appeals Department – Medicaid/MIChild
UnitedHealthcare Community and State
P.O. Box 2127
Southfield, MI 48037
Mail all UnitedHealthcare Community Plan Dual Complete Provider Appeal requests to:
Provider Appeals Department - Dual Complete
UnitedHealthcare Community and State
P.O. Box 2127
Southfield, MI 48037
Please refer to the following disclaimer about the use of the UnitedHealthcare Claim Reconsideration Request Form.
You may have additional rights under state law. For review of claims for members enrolled in other benefit plans, please refer to one or more of the following for information on requesting claim reviews: the Web site for the entity on the member's health care ID card, the EOB for the applicable claim, or UnitedHealthcareOnline.com. You may also call the telephone number on the member's health care ID card for information on how to request claims review.