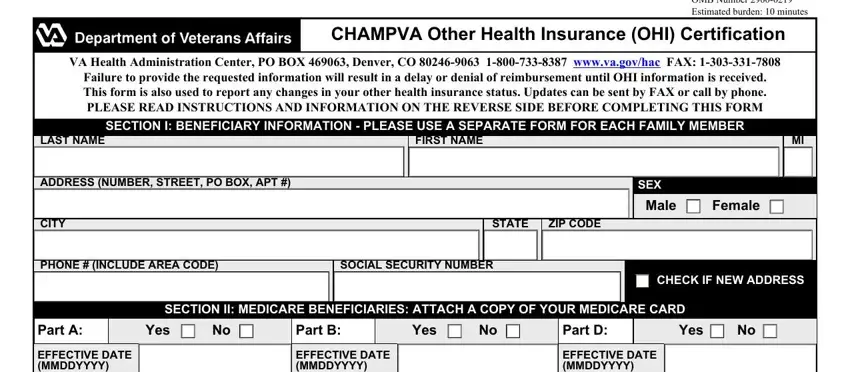
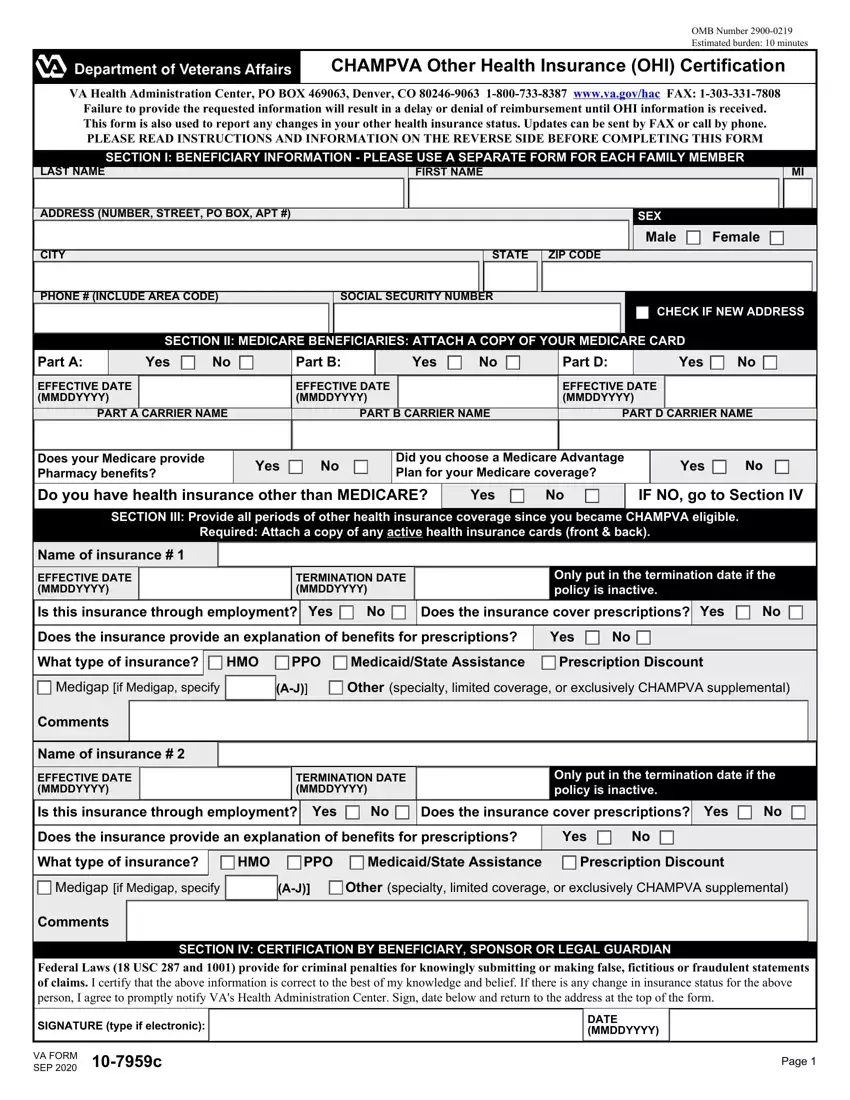
CHAMPVA OTHER HEALTH INSURANCE (OHI) CERTIFICATION
NOTES, DEFINITIONS, AND INSTRUCTIONS
INSTRUCTIONS
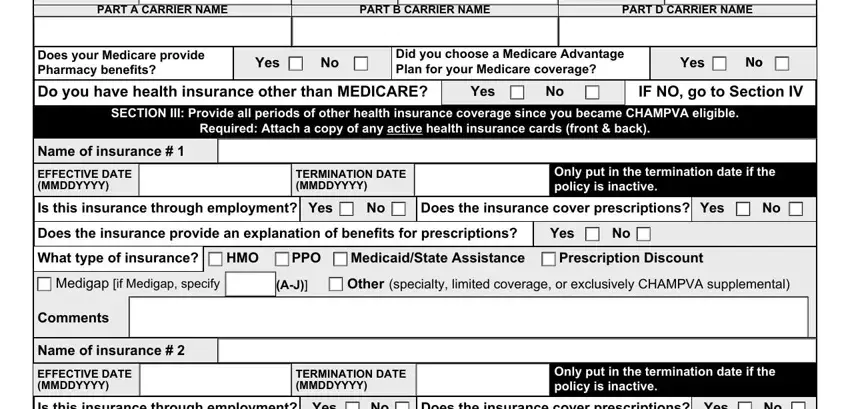
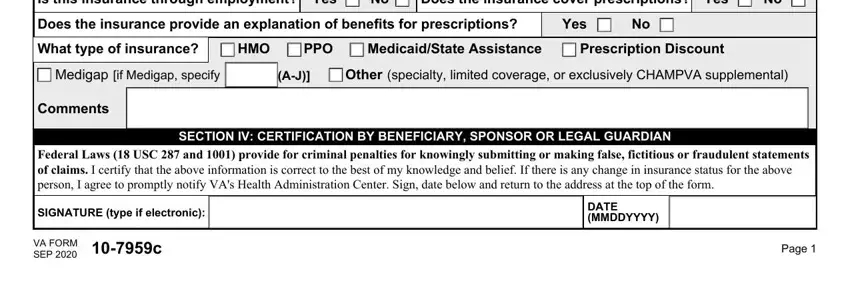
Failure to complete all applicable sections on the front can result in a delay or denial of benefits. Use this form to report any changes in your other health insurance.
•New beneficiaries - we need OHI information from the date your CHAMPVA eligibility became effective.
•Re-certification - update OHI information every time a change is made to your OHI coverage.
•To specify a medicare supplement plan A - J, refer to your policy cover sheet or your insurance membership card.
•If there are additional policies use plain bond paper and either type or legibly print your name, SSN, and the information for each item. Attach to this form. If submitting this form electronically add an attachment to the submission.
ITEMS TO RETURN WITH THIS COMPLETED OTHER HEALTH INSURANCE (OHI) CERTIFICATION
•A COPY of your Medicare card (do NOT send the original)
•A COPY of your other health insurance (OHI) member ID card (front and back).
•If your OHI does not issue EOBs, then attach a copy (card or document) of your schedule of benefits that lists your co-payments.
DEFINITIONS
OHI: OHI refers to insurance or benefits you may have other than CHAMPVA called “Other Health Insurance”.
EOB: The abbreviation for an “explanation of benefits” form or letter that must accompany claims submitted to CHAMPVA. An EOB is a statement or “Remittance Advice” from an insurance carrier or benefit program that summarizes the action taken on a claim.
Note: If you have OHI primary to CHAMPVA you must submit EOB's for each primary insurance along with health care claims. If your OHI does not issue EOB's i.e. some HMO's and PPO's, you must submit a copy of your active co-payment information shown on your insurance card or a document showing your co-payments with every health care claim so CHAMPVA can calculate benefit payments.
Carrier: Carrier is the insurance company that provides your medical benefits.
OHI primary to CHAMPVA: CHAMPVA by law is always supplemental or the secondary payer of health care benefits except for Medicaid, State Victims of Crimes Compensation Programs, and policies purchased exclusively to supplement CHAMPVA benefits.
Supplemental CHAMPVA policies: These are policies specifically purchased for the purpose of covering your cost share after CHAMPVA has completed adjudication of a claim.
Medicare supplemental policies: These are policies that are specifically for the purpose of covering your Medicare out of pocket expenses. These Medicare supplemental policies such as “Medigap” or Policies offered through employment are primary to CHAMPVA and must provide an EOB along with the Medicare EOB (two EOBs) for each claim submitted to CHAMPVA.
Indemnity: Plans that pay a flat fee or daily rate to supplement lost income while hospitalized are called Indemnity Plans.
Termination date: This is the date the policy ended or ceased to be active. The end date for a period shown on a card that will be reissued is not the termination date. Closing a policy will generate a true termination date.
Privacy Act Information: The authority for collection of the requested information on this form is 38 USC 501 and 1781. The purpose of collecting this information is to determine payer status when other health insurance coverage exists. The information you provide may be verified by a computer matching program at any time. You are requested to provide your Social Security number as your VA record is filed and retrieved by this number. You do not have to provide the requested information on this form but if any or all of the requested information is not provided, it may delay or result in denial of your request for CHAMPVA benefits. Failure to furnish the requested information will have no adverse impact on any other VA benefit to which you may be entitled. The responses you submit are considered confidential and may be disclosed outside VA only if the disclosure is authorized under the Privacy Act, including the routine uses identified in the VA system of records number 54VA16, titled "Health Administration Center Civilian Health and Medical Program Records -VA", as set forth in the Compilation of Privacy Act Issuances via online GPO access at http://www.gpoaccess.gov/privacyact/index.html. For example, information including your Social Security number may be disclosed to contractors, trading partners, health care providers and other suppliers of health care services to determine your eligibility for medical benefits and payment for services.
Paperwork Reduction Act: This information collection is in accordance with the clearance requirements of Section 3507 of the Paperwork Reduction Act of 1995. Public reporting burden for this collection of information is estimated to average 10 minutes per response, including the time for reviewing instructions, searching existing data sources, gathering and maintaining the data needed, and completing and reviewing the collection of information. Comments regarding this burden estimate or any other aspect of this collection, including suggestions for reducing the burden, may be addressed by calling the CHAMPVA Help Line, 800-733-8387. Respondents should be aware that notwithstanding any other provision of law, no person shall be subject to any penalty for failing to comply with a collection of information if it does not display a currently valid OMB control number. This collection of information is to determine payer status when other health insurance coverage exists.
 Female
Female 
 No
No N
N No
No