When you want to fill out physical exam forms, you don't need to download any kind of software - simply give a try to our online PDF editor. The editor is consistently maintained by our staff, receiving new awesome functions and becoming better. Getting underway is simple! All you should do is adhere to the following simple steps down below:
Step 1: Access the PDF form in our tool by pressing the "Get Form Button" above on this webpage.
Step 2: This editor will allow you to work with PDF documents in many different ways. Improve it by including your own text, adjust existing content, and place in a signature - all readily available!
This form will need specific details; to guarantee accuracy and reliability, don't hesitate to heed the next tips:
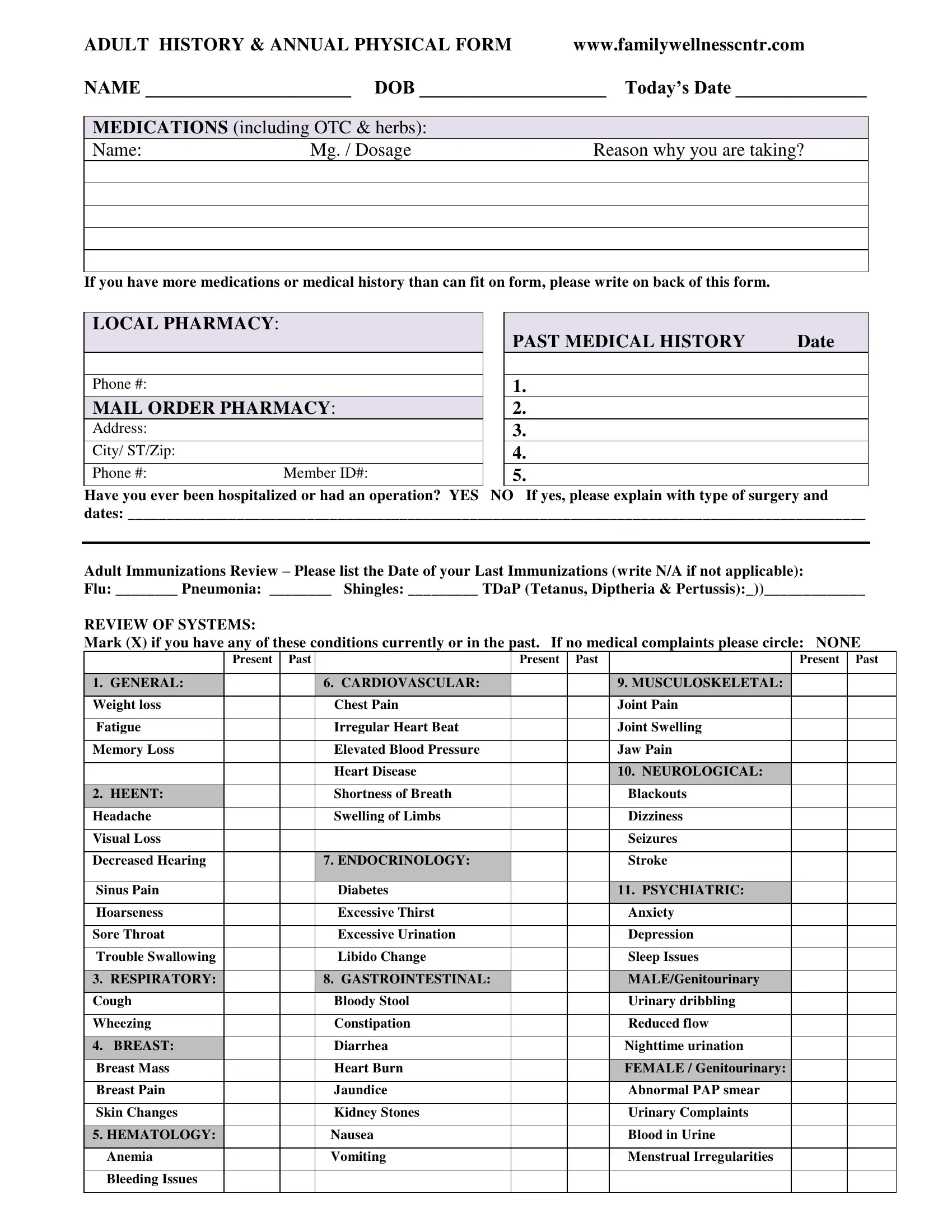
1. Start completing your physical exam forms with a selection of major blanks. Consider all the necessary information and ensure there's nothing left out!
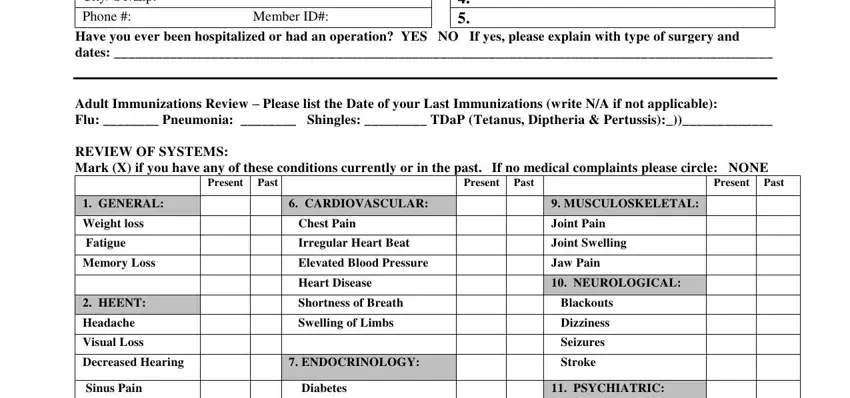
2. The next part would be to fill in the next few fields: City STZip, Phone Member ID, Have you ever been hospitalized or, Adult Immunizations Review Please, GENERAL, Weight loss, Fatigue, Memory Loss, HEENT, Headache, Visual Loss, Decreased Hearing, Sinus Pain, Present Past, and CARDIOVASCULAR.
3. This next portion is all about Hoarseness, Sore Throat, Trouble Swallowing, RESPIRATORY, Cough, Wheezing, BREAST, Breast Mass, Breast Pain, Skin Changes, HEMATOLOGY, Anemia, Bleeding Issues, Excessive Thirst, and Excessive Urination - fill out every one of these empty form fields.
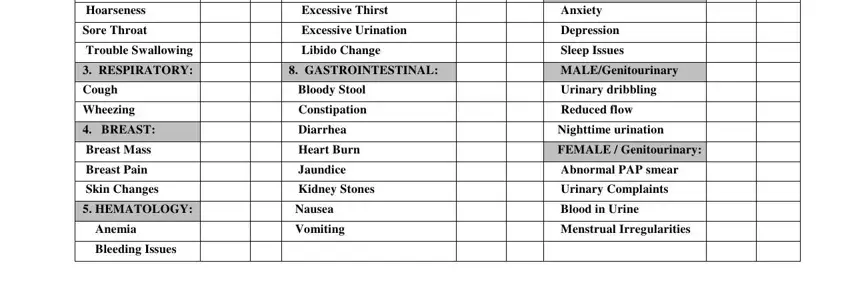
It's easy to make errors while filling in the Breast Mass, and so make sure you take a second look before you finalize the form.
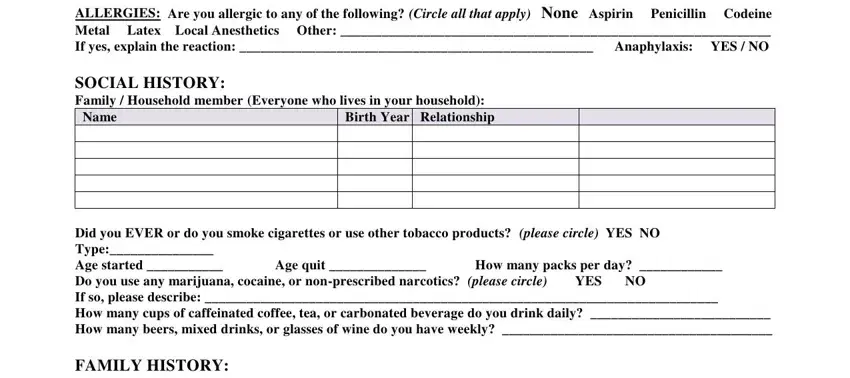
4. To go ahead, the next stage involves filling in a couple of form blanks. Included in these are ALLERGIES Are you allergic to any, Name, Birth Year Relationship, Age quit , How many packs per day , and Did you EVER or do you smoke, which are essential to continuing with this PDF.
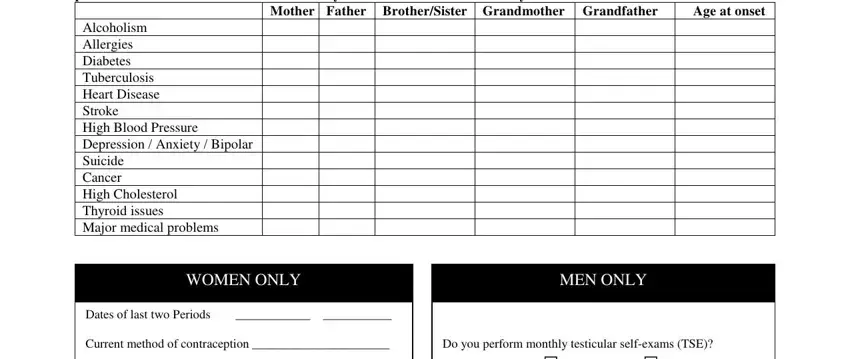
5. Because you approach the final sections of this file, you will find just a few more things to undertake. Notably, Did you EVER or do you smoke, Mother Father BrotherSister, Age at onset, WOMEN ONLY, Dates of last two Periods Current, MEN ONLY, Do you perform monthly testicular, and Yes should all be filled out.
Step 3: Reread everything you've entered into the blanks and then press the "Done" button. Get your physical exam forms after you subscribe to a 7-day free trial. Quickly get access to the pdf file inside your FormsPal cabinet, with any edits and changes being conveniently kept! We do not share or sell the information that you enter while dealing with forms at our website.