Follow the steps below to properly complete this annual physical examination form in PDF format.
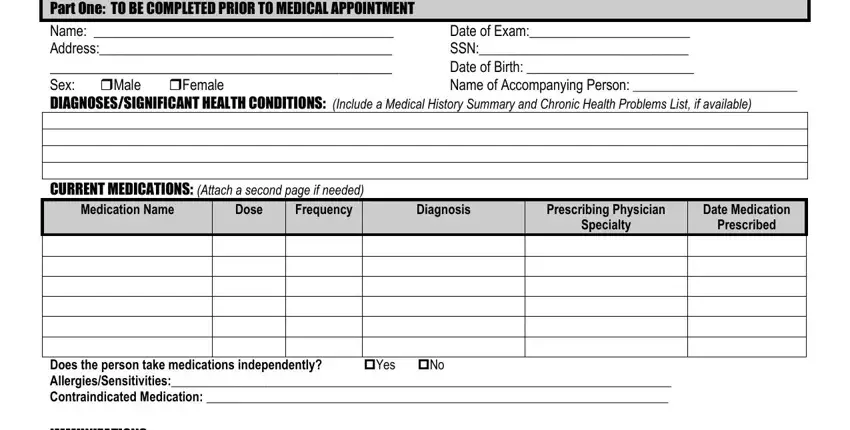
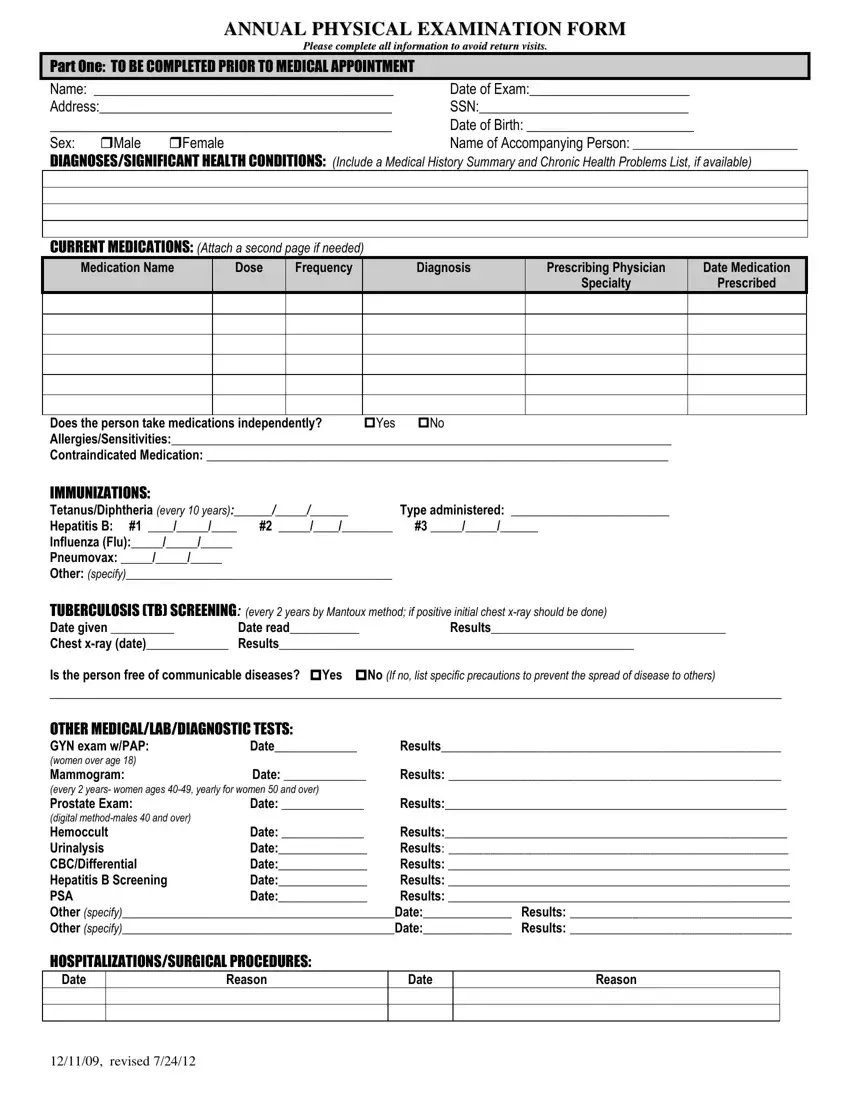
1. Pre-Appointment Section
Start with Part One before the medical visit:
- Fill in the individual’s name, address, date of birth, exam date, and other identifying details.
- From there, list current diagnoses and health conditions, along with medications, allergies, and any contraindicated medications.
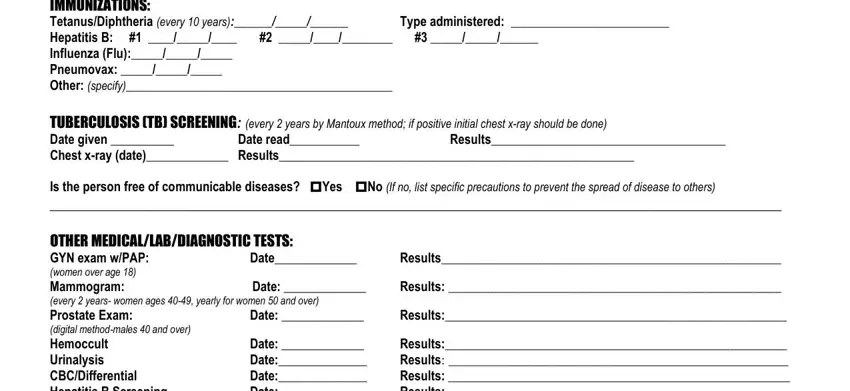
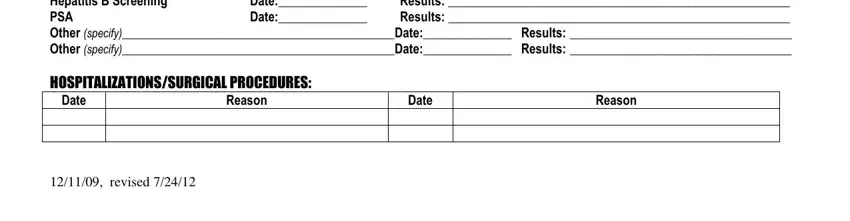
- After that, add immunization dates, tuberculosis screening results, and information about past hospitalizations or surgeries.
If something does not apply, make that clear instead of leaving the space blank.
2. Supporting Details
Before the appointment, review medication lists, lab results, and prior records for accuracy. Add extra pages if the medication or medical history sections need more space.
Double-check dates and prescribing details, since even small inconsistencies can lead to follow-up requests from agencies or reviewers.
3. Physical Examination
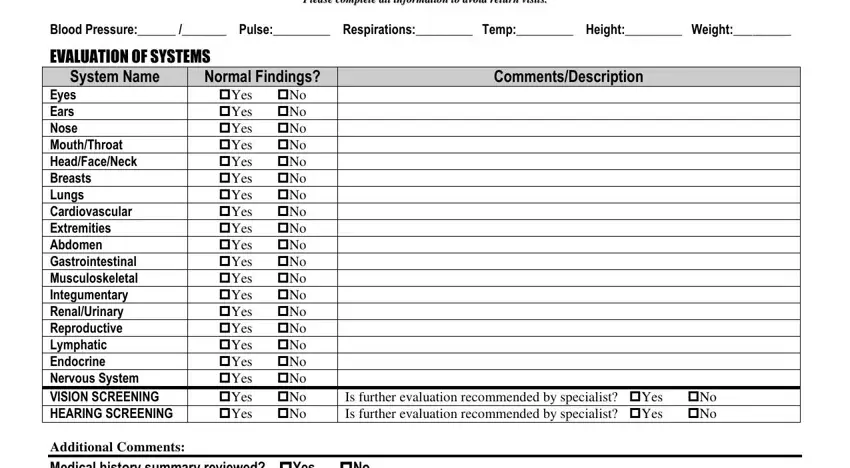
During the appointment, the physician completes Part Two of this annual physical exam form template. This section covers vital signs, system-by-system findings, vision and hearing screenings, and any relevant comments.
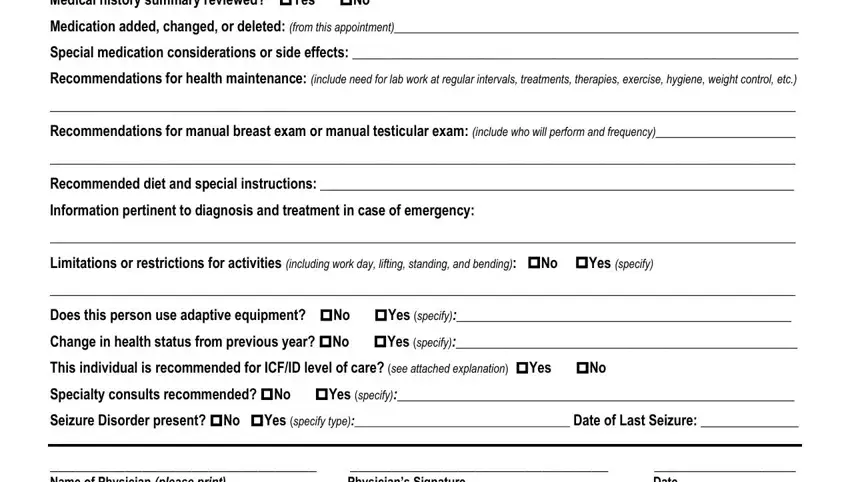
The physician should note any changes since the prior year, record activity limits or use of adaptive equipment, and clearly document recommendations for care, referrals, or follow-up.
4. Required Certifications
The physician should answer every yes-or-no question related to health status, level of care, specialty consults, and seizure disorders when applicable.
Each response must align with the clinical notes to avoid conflicting or unclear information.
5. Final Part
The physician should print and sign their name, add the date, and include contact information.
Keep the completed form on file as part of the individual’s medical record.