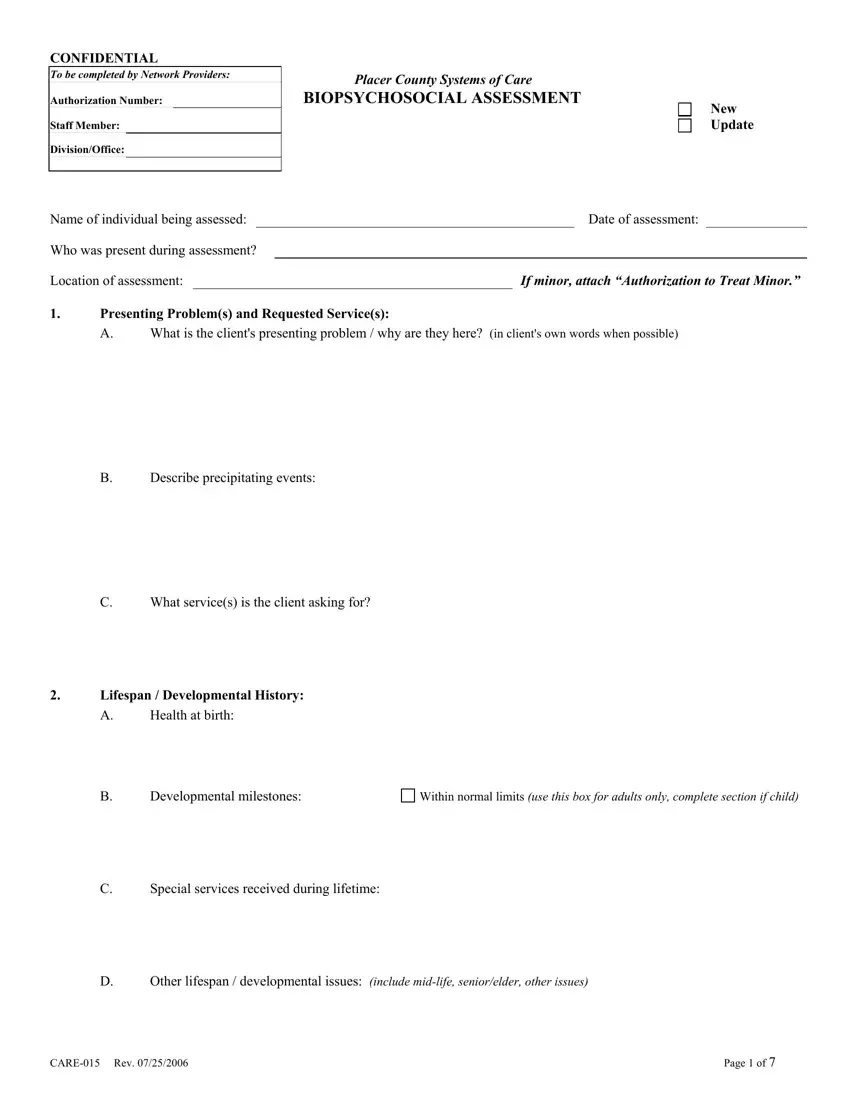
There isn't anything complex regarding working with the biopsychosocial assessment template social work pdf once you open our PDF editor. By following these basic steps, you'll get the prepared PDF within the minimum time possible.
Step 1: Discover the button "Get Form Here" and press it.
Step 2: Now you are going to be on your form edit page. You can add, customize, highlight, check, cross, add or erase fields or phrases.
For each section, prepare the data required by the system.
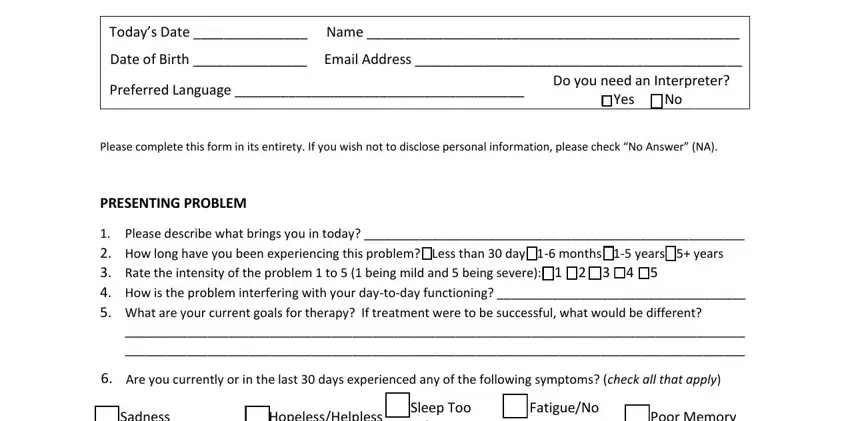
The program will expect you to fill out the Sadness, HopelessHelpless, No Motivation, Lack of Interest, Not Hungry, Prefer Being Alone, Sleep Too Much Thoughts of Dying, No Need for Sleep, Talk Too Fast, Impulsive, Suspicious, Hearing Things, Seeing Things, FatigueNo Energy, and Guilt part.
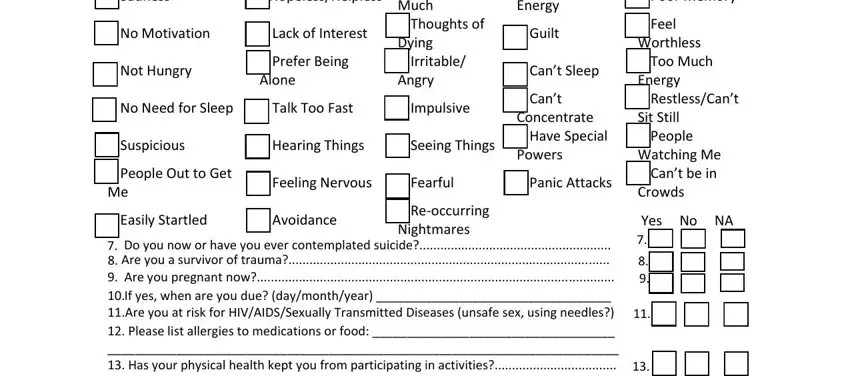
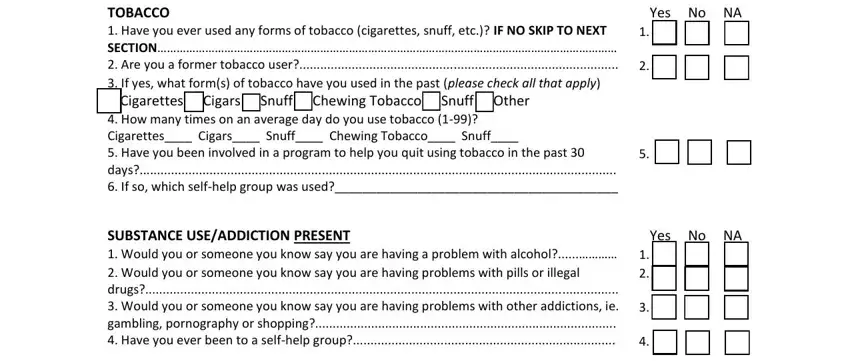
You'll be required particular important details to be able to submit the TOBACCO Have you ever used any, Yes No NA, SUBSTANCE USEADDICTION PRESENT, and Yes No NA box.
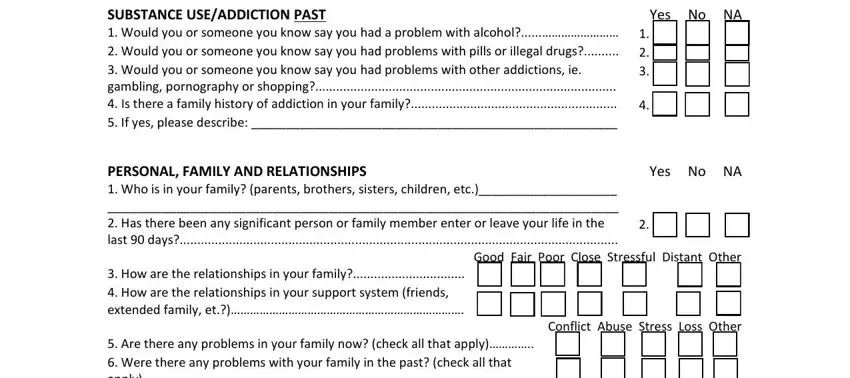
For field SUBSTANCE USEADDICTION PAST Would, Yes No NA, PERSONAL FAMILY AND RELATIONSHIPS, Yes No, Good Fair Poor Close Stressful, How are the relationships in your, Are there any problems in your, and Conflict Abuse Stress Loss Other, state the rights and obligations.
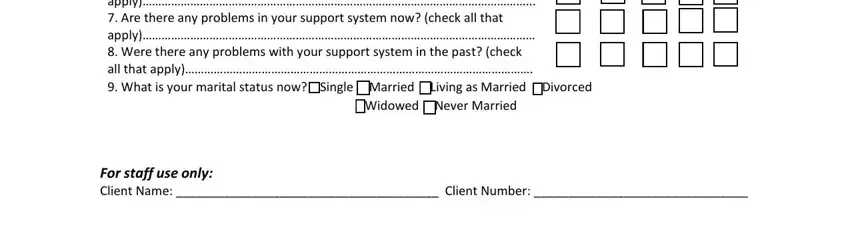
End by reading the following areas and writing the suitable data: Are there any problems in your, Widowed Never Married, and For staff use only Client Name.
Step 3: Hit the button "Done". The PDF document can be exported. You will be able download it to your computer or send it by email.
Step 4: In order to prevent possible upcoming concerns, it is important to have at the very least several duplicates of every single document.