When using the online tool for PDF editing by FormsPal, you're able to fill out or alter Washington here. FormsPal is devoted to providing you the best possible experience with our editor by constantly introducing new capabilities and upgrades. Our tool is now a lot more user-friendly thanks to the latest updates! Currently, filling out documents is simpler and faster than ever. To start your journey, go through these basic steps:
Step 1: Just click on the "Get Form Button" above on this page to see our form editor. There you will find everything that is needed to work with your document.
Step 2: The editor gives you the ability to modify almost all PDF forms in a variety of ways. Enhance it by writing customized text, correct original content, and put in a signature - all at your convenience!
This PDF form requires some specific details; to guarantee consistency, you should heed the next tips:
1. First of all, when completing the Washington, start in the form section containing following blank fields:
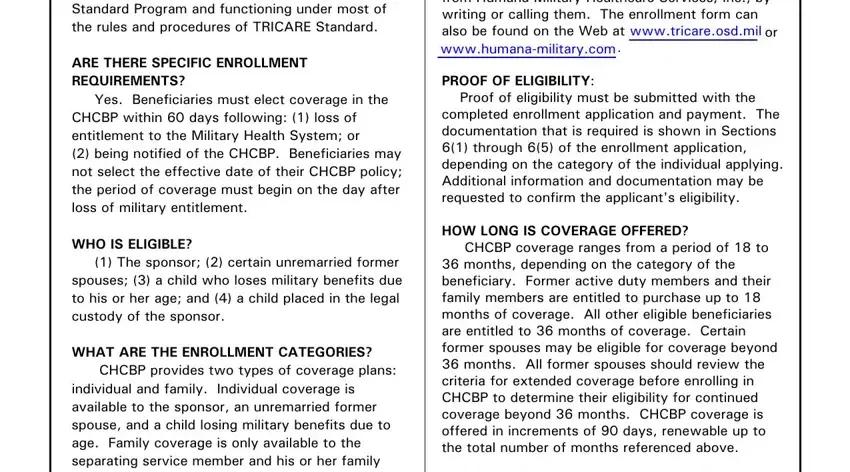
2. Once your current task is complete, take the next step – fill out all of these fields - claim Information regarding where, Write or call, can be found at the TRICARE Web, wwwtricareosdmil or by contacting, Humana Military Healthcare, Military Healthcare Services Inc, Attn CHCBP, Center nearest the enrollees, PO Box, Louisville KY, If there are any problems with the, CHCBP claim the enrollee should, processor If that is not, then write to the TRICARE, and or visit their Web Site at with their corresponding information. Make sure to double check that everything has been entered correctly before continuing!
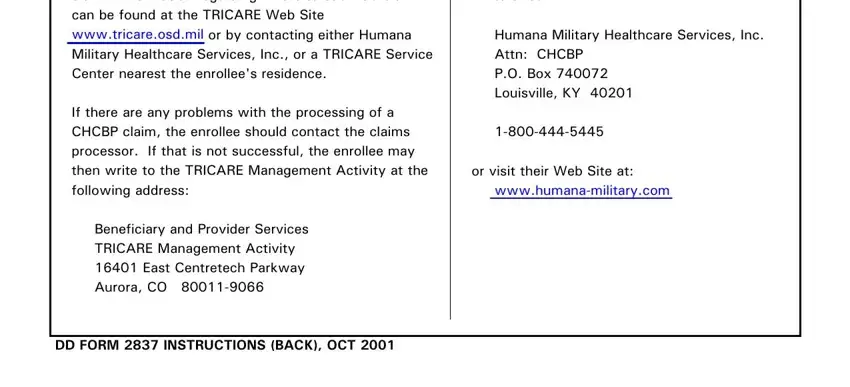
3. The following segment is about CONTINUED HEALTH CARE BENEFIT, APPLICATION, Form Approved OMB No Expires Jun, The public reporting burden for, PRIVACY ACT STATEMENT, AUTHORITY USC and EO PRINCIPAL, APPLICANT NAME Last First Middle, TELEPHONE NO Include Area Code, RESIDENCE ADDRESS Street, MAILING ADDRESS If different from, a HOME, b WORK, SERVICE MEMBER SPONSOR THROUGH, a NAME Last First Middle Initial, and b SPONSORS SOCIAL SECURITY NUMBER - complete these blank fields.
People generally get some things incorrect while filling in MAILING ADDRESS If different from in this part. Ensure that you go over whatever you type in here.
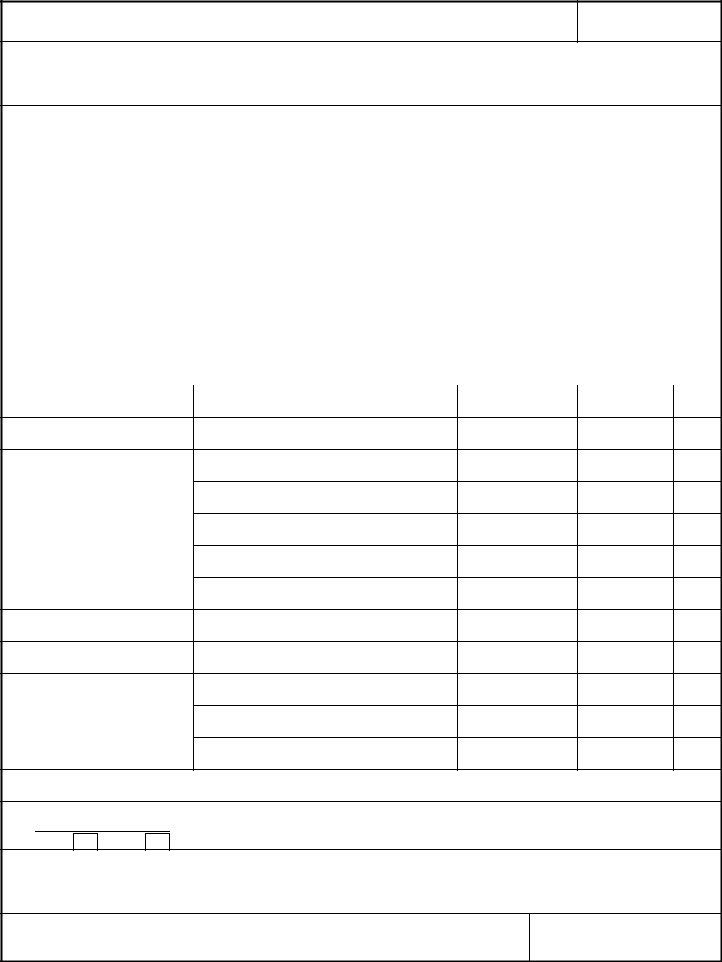
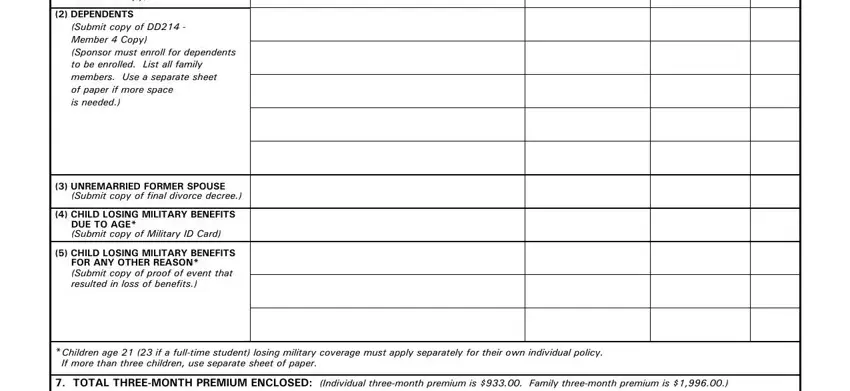
4. This next section requires some additional information. Ensure you complete all the necessary fields - SPONSOR Submit copy of DD Member, DEPENDENTS Submit copy of DD, UNREMARRIED FORMER SPOUSE Submit, CHILD LOSING MILITARY BENEFITS, CHILD LOSING MILITARY BENEFITS, Children age if a fulltime, and TOTAL THREEMONTH PREMIUM ENCLOSED - to proceed further in your process!
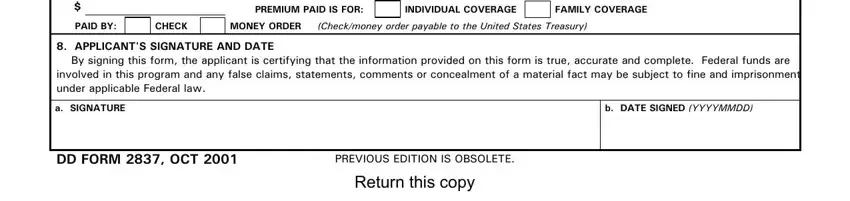
5. As you draw near to the last parts of your form, you will find a few extra points to do. Mainly, TOTAL THREEMONTH PREMIUM ENCLOSED, INDIVIDUAL COVERAGE, PREMIUM PAID IS FOR, FAMILY COVERAGE, PAID BY, CHECK, MONEY ORDER Checkmoney order, APPLICANTS SIGNATURE AND DATE By, a SIGNATURE, b DATE SIGNED YYYYMMDD, DD FORM OCT, PREVIOUS EDITION IS OBSOLETE, and Return this copy must all be done.
Step 3: After taking one more look at your completed blanks, click "Done" and you're all set! Join FormsPal now and instantly get Washington, ready for download. Every last edit made is handily saved , which means you can edit the form later on when necessary. FormsPal provides safe document editing with no data recording or sharing. Rest assured that your information is in good hands with us!