This PDF editor was designed to be as straightforward as it can be. As you keep up with the following actions, the procedure for filling out the Dma 5003 form will be straightforward.
Step 1: You can click the orange "Get Form Now" button at the top of the webpage.
Step 2: After you have accessed the editing page Dma 5003, you'll be able to find each of the options available for the form within the top menu.
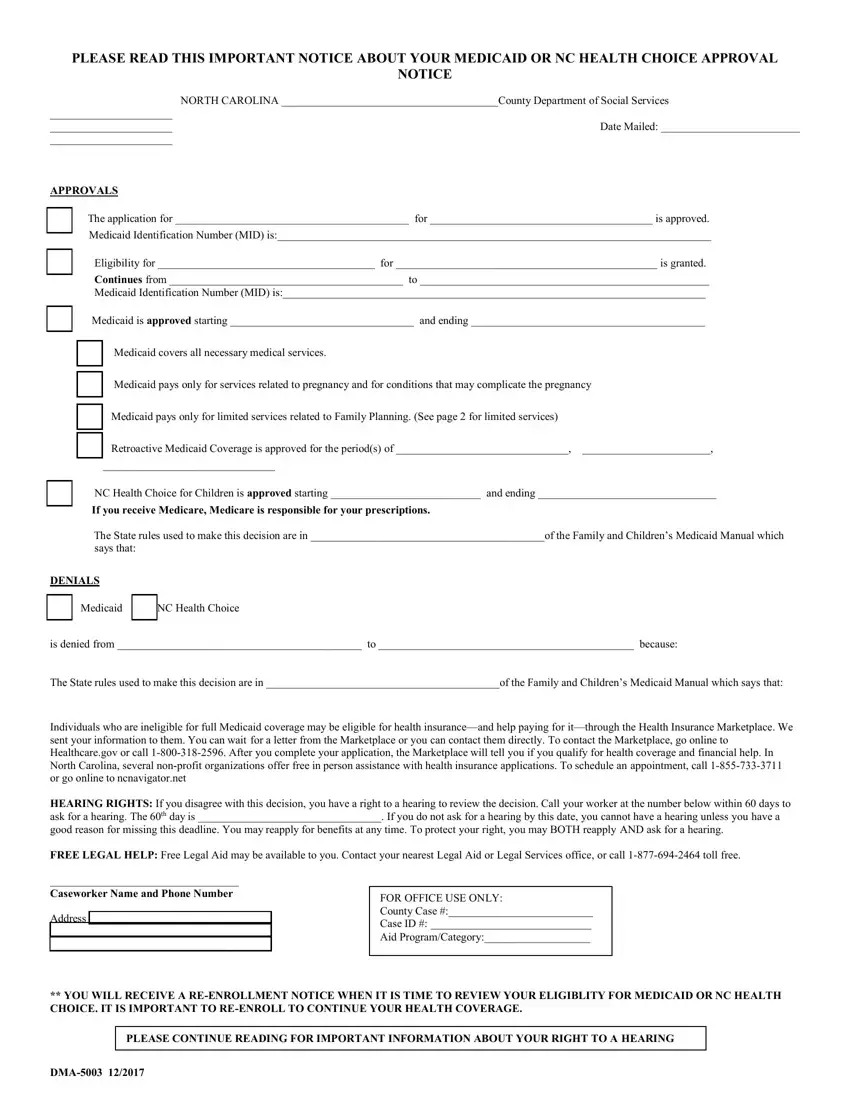
You will have to enter the next information if you want to fill out the file:
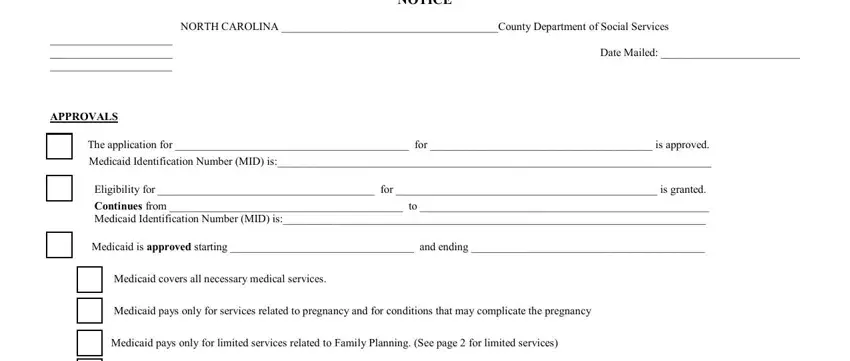
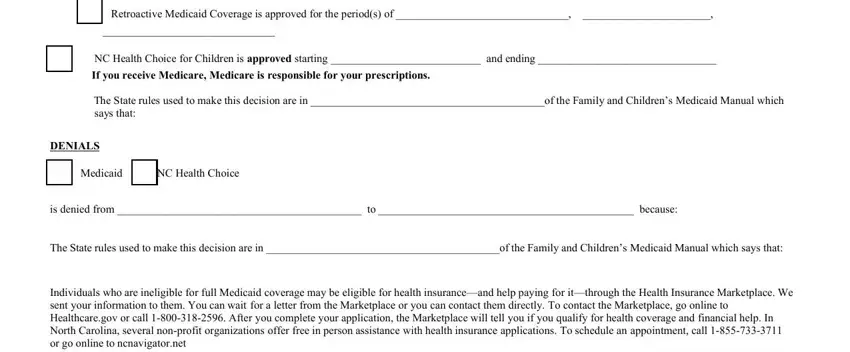
Fill in the Medicaid covers all necessary, NC Health Choice for Children is, If you receive Medicare Medicare, The State rules used to make this, DENIALS, Medicaid NC Health Choice, is denied from to because, The State rules used to make this, and Individuals who are ineligible for areas with any particulars that will be required by the software.
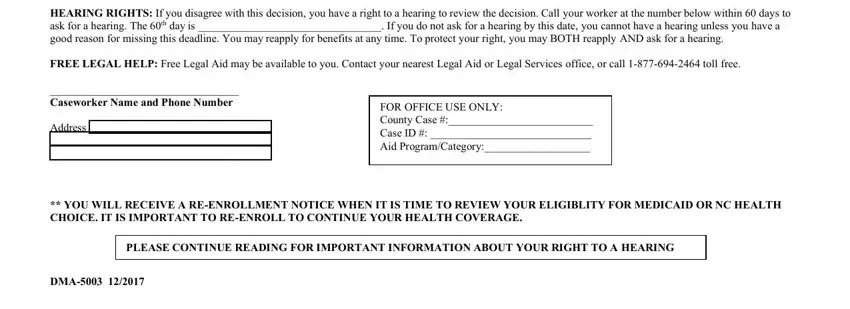
You'll be asked to note the information to let the program fill in the part HEARING RIGHTS If you disagree, FREE LEGAL HELP Free Legal Aid may, Caseworker Name and Phone Number, Address, FOR OFFICE USE ONLY County Case, YOU WILL RECEIVE A REENROLLMENT, PLEASE CONTINUE READING FOR, and DMA.
Step 3: Once you've hit the Done button, your form is going to be available for transfer to each device or email address you specify.
Step 4: Be certain to avoid potential problems by making a minimum of 2 copies of the document.