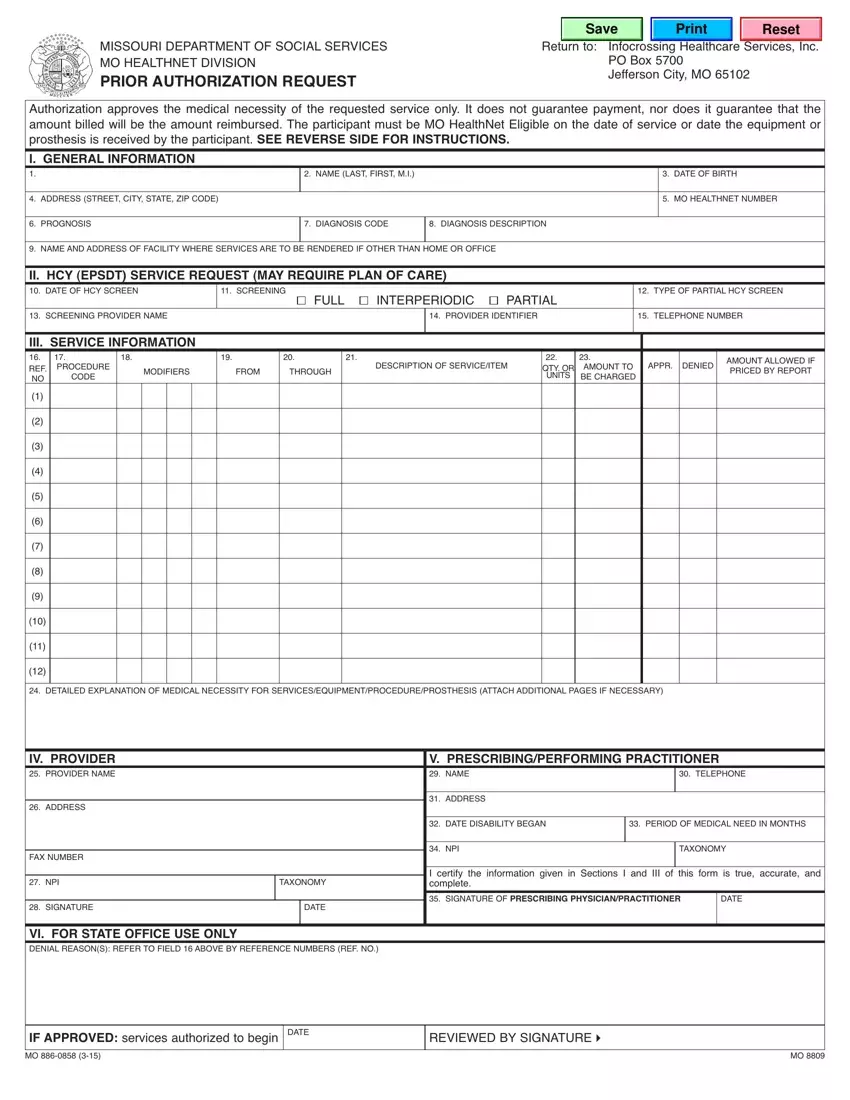
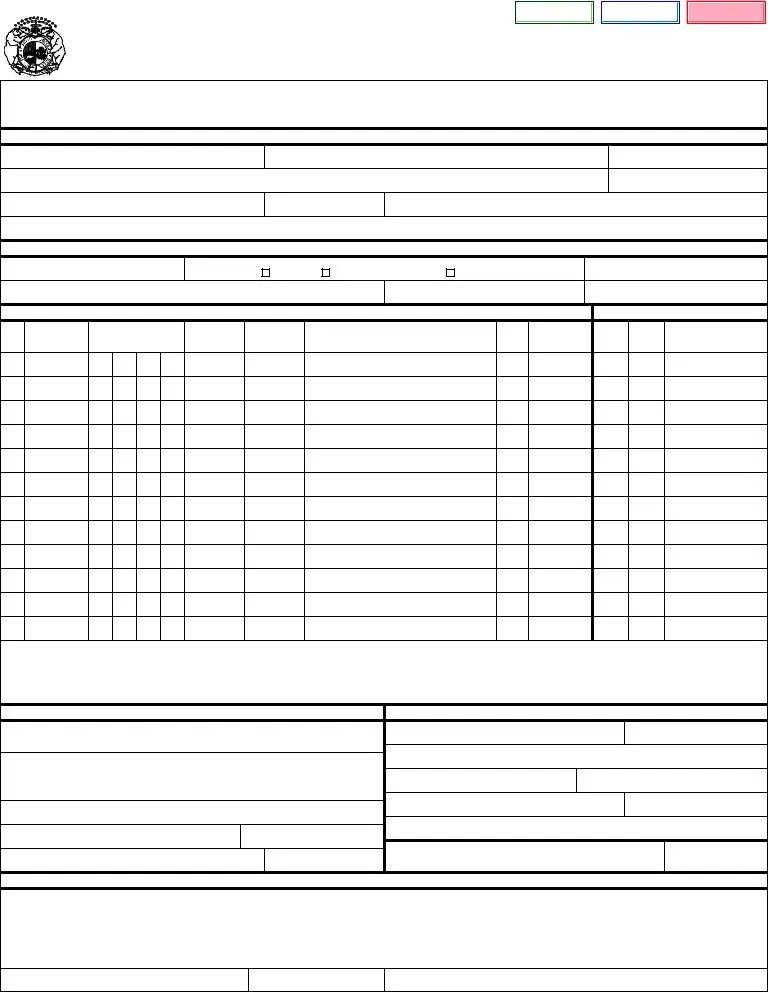
INSTRUCTIONS FOR COMPLETION
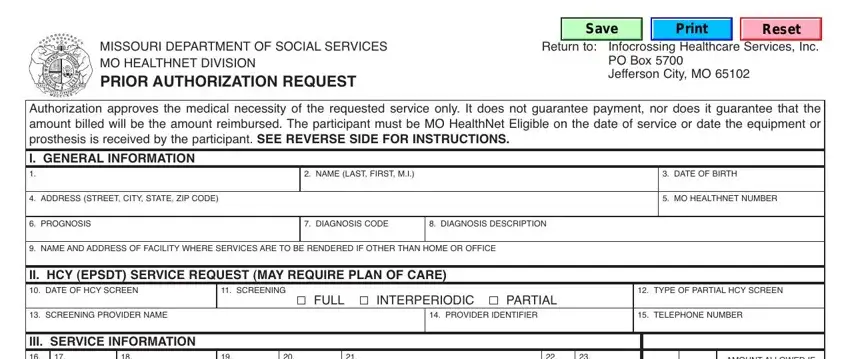
I. GENERAL INFORMATION - To be completed by the provider requesting the prior authorization. 1. leave blank
2. participant’s name - enter the participant’s name as it appears on the mo healthnet id card. enter the participant’s current address.
3. date of birth - enter the participant’s date of birth.
4. address - enter the participant’s address, city, state, and zip.
5. mo healthnet number - enter the participant’s 8-digit mo healthnet identification number as shown on the mo healthnet identification card or county letter of eligibility.
6. prognosis - enter the participant’s prognosis.
7. diagnosis code - enter the diagnosis code(s).
8. diagnosis description - enter the diagnosis description. if there is more than one diagnosis, enter all descriptions appropriate to the services being requested.
9. name and address of the facility where services are to be rendered if service is to be provided other than home or office.
II. HCY SERVICE REQUEST (Plan of care may be required, see your provider manual) 10. date of hcy screen - enter the date the hcy screen was done.
11. screening - check whether the screening performed was full, interperiodic, or partial.
12. type of partial hcy screen - enter the type of partial hcy screen that was performed. (e.g., vision, hearing, etc.)
13. screening provider name - enter the provider’s name who performed the screening.
14. provider identifier - enter the provider’s npi number who performed the screening.
15. telephone number - enter the screening provider’s telephone number including the area code.
III. SERVICE INFORMATION
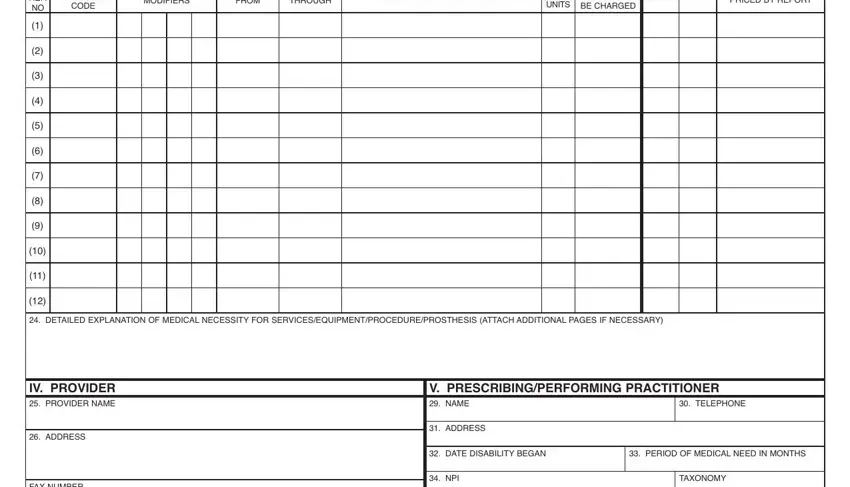
16. ref. no. - (reference number) a unique designator (1-12) identifying each separate line on the request.
17. procedure code - enter the procedure code(s) for the services being requested.
18. modifier - enter the appropriate modifier(s) for the services being requested.
19. from - enter the from date that services will begin if authorization is approved (mm/dd/yy format).
20. through - enter the through date the services will terminate if authorization is approved (mm/dd/yy format).
21. description of service/item - enter a specific description of the service/item being requested.
22. quantity or units - enter the quantity or units of service/item being requested.
23. amount to be charged - enter the amount to be charged for the service.
24. detailed explanation of medical necessity of the service, equipment/procedure/prosthesis, etc. attach additional page(s) as necessary.
Do not use another Prior Authorization Form.
IV. PROVIDER REQUESTING PRIOR AUTHORIzATION
25. provider name - enter the requested provider’s information. if a clinic or group practice, also complete section v.
26. address - enter the complete mailing address in this field.
27. npi - enter the provider’s npi and taxonomy code (if applicable).
28. signature/date - the provider of services should sign the request and indicate the date the form was completed. (check your provider manual to determine if this field is required.)
V. PRESCRIBING/PERFORMING PRACTITIONER
this section must be completed for services which require a prescription such as durable medical equipment, physical therapy, or for services which will be prescribed by a physician/practitioner that require prior authorization, or when the provider in section iv is a clinic or group practice. check your provider manual for additional instructions.
29. name - enter the name of the prescribing/performing practitioner.
30. telephone number - enter the prescribing/performing practitioner telephone number including area code.
31. address - enter the address, city, state, and zip code.
32. date disability began - enter the date the disability began. for example, if a disability originated at birth, enter date of birth.
33. period of medical need in months - enter the estimated number of months the participant will need the equipment/services.
34. npi - enter the provider’s npi and taxonomy code (if applicable).
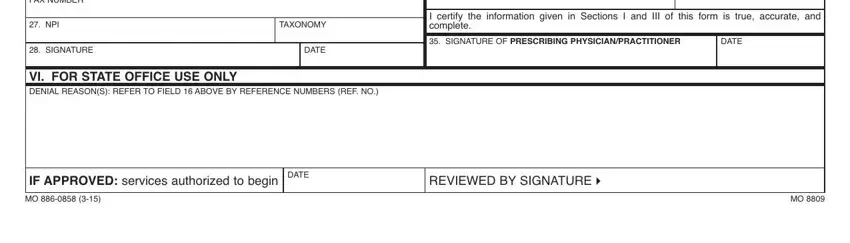
35. signature of prescribing/performing practitioner - the prescribing physician/practitioner must sign and indicate the date signed in mm/dd/yy format. (Signature stamps are not acceptable)
VI. FOR STATE OFFICE USE ONLY
approval or denial for each line will be indicated in the box to the right of section iii. also in this box the consultant will indicate allowed amount if procedure requires manual pricing.
at the bottom, the consultant may explain denials or make notations referencing the specific procedure code and description by number (1 thru 12). the consultant will sign or initial the form.