TO THE PROVIDER - REQUEST FOR APPROVAL TO VARY FROM MEDICAL TREATMENT GUIDELINES
1.This form is used for a workers' compensation, volunteer firefighters' or volunteer ambulance workers' benefit case as follows: To request approval to vary the treatment of the patient identified on this form from the relevant Medical Treatment Guidelines.
2.This form must be signed by the Treating Medical Provider and must contain his/her authorization number and code letters. Out-of-State medical providers must enter their NPI number. If the patient is hospitalized, it may be signed by a licensed doctor to whom the treatment of the case has been assigned as a member of the attending staff of the hospital.
3.Please ask your patient for his/her WCB case number and the claim administrator claim (carrier case) number and show these numbers on the form. In addition, ask your patient if he/she has retained a representative. If represented, ask for the name and address of the representative.
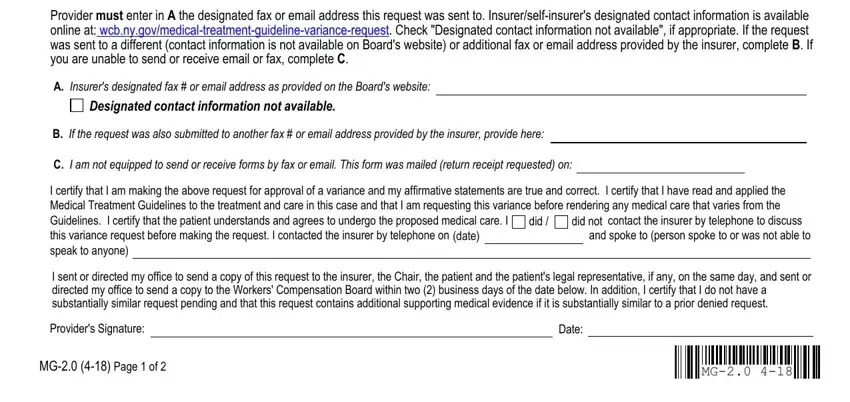
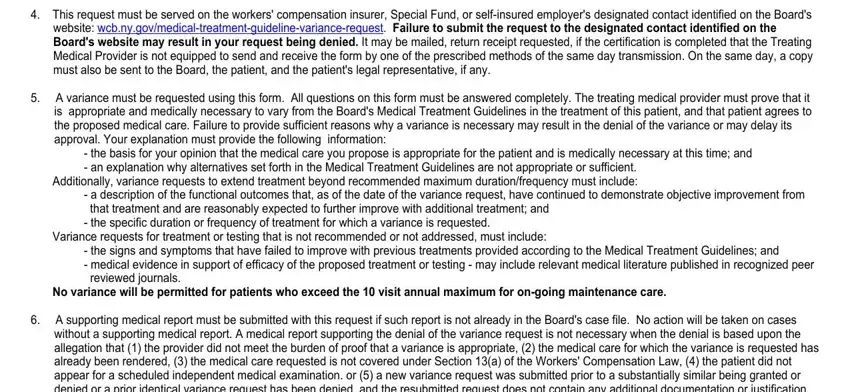
4.This request must be served on the workers' compensation insurer, Special Fund, or self-insured employer's designated contact identified on the Board's website: wcb.ny.gov/medical-treatment-guideline-variance-request. Failure to submit the request to the designated contact identified on the Board's website may result in your request being denied. It may be mailed, return receipt requested, if the certification is completed that the Treating Medical Provider is not equipped to send and receive the form by one of the prescribed methods of the same day transmission. On the same day, a copy must also be sent to the Board, the patient, and the patient's legal representative, if any.
5.A variance must be requested using this form. All questions on this form must be answered completely. The treating medical provider must prove that it is appropriate and medically necessary to vary from the Board's Medical Treatment Guidelines in the treatment of this patient, and that patient agrees to the proposed medical care. Failure to provide sufficient reasons why a variance is necessary may result in the denial of the variance or may delay its approval. Your explanation must provide the following information:
-the basis for your opinion that the medical care you propose is appropriate for the patient and is medically necessary at this time; and
-an explanation why alternatives set forth in the Medical Treatment Guidelines are not appropriate or sufficient.
Additionally, variance requests to extend treatment beyond recommended maximum duration/frequency must include:
-a description of the functional outcomes that, as of the date of the variance request, have continued to demonstrate objective improvement from that treatment and are reasonably expected to further improve with additional treatment; and
-the specific duration or frequency of treatment for which a variance is requested.
Variance requests for treatment or testing that is not recommended or not addressed, must include:
-the signs and symptoms that have failed to improve with previous treatments provided according to the Medical Treatment Guidelines; and
-medical evidence in support of efficacy of the proposed treatment or testing - may include relevant medical literature published in recognized peer reviewed journals.
No variance will be permitted for patients who exceed the 10 visit annual maximum for on-going maintenance care.
6.A supporting medical report must be submitted with this request if such report is not already in the Board's case file. No action will be taken on cases without a supporting medical report. A medical report supporting the denial of the variance request is not necessary when the denial is based upon the allegation that (1) the provider did not meet the burden of proof that a variance is appropriate, (2) the medical care for which the variance is requested has already been rendered, (3) the medical care requested is not covered under Section 13(a) of the Workers' Compensation Law, (4) the patient did not appear for a scheduled independent medical examination. or (5) a new variance request was submitted prior to a substantially similar being granted or denied or a prior identical variance request has been denied, and the resubmitted request does not contain any additional documentation or justification.
7.If approval or denial is not forthcoming within 15 calendar days after the insurer has received the request and an IME or Medical Record Review is not required, the variance is deemed approved and the Board will issue an Order of the Chair stating the request is approved. If the insurer decides either an IME or records review is required, the insurer must notify the Board and Treating Medical Provider within 5 business days that it will be obtaining an outside opinion. The insurer has 30 calendar days to get the IME exam or Medical Records Review and submit Form IME-4. If no notice of an IME or Medical Record Review is submitted, the insurer has 15 calendar days from the date of the request to reply to the variance request.
8.If the claim is controverted, the Treating Medical Provider must request approval for the variance from the insurer or Special Fund who would be responsible if the claim is established using this form and process.
9.If the insurer has checked "GRANTED" or "GRANTED IN PART" AND "WITHOUT PREJUDICE" in Section E, the liability for this claim has not yet been determined. This authorization is made pending final determination by the Board. Pursuant to 12 NYCRR § 324.3(b)(4), this authorization is limited to the question of medical necessity only and is not an admission that the condition for which the services are required is compensable. This authorization does not represent an acceptance of this claim by the insurer, self-insured employer, employer or Special Fund or guarantee payment for the services authorized. When a decision is rendered regarding liability, you will receive a Notice of Decision by mail. The insurer, self-insured employer, employer or Special Fund will only provide payment for these services if the claim is established and the insurer, self-insured employer, employer or Special Fund is found to be responsible for the claim.
10.If the insurer has checked "SUBSTANTIALLY SIMILAR REQUEST PENDING OR DENIED" in Section E, the denial is not subject to an Order of the Chair. A substantially similar variance request may not be submitted unless the insurer has denied a previous request. Substantially similar requests that were previously denied may be submitted with additional documentation or justification.
11.Treating Medical Providers, which includes any physician, podiatrist, chiropractor or psychologist who is providing treatment and care to an injured worker pursuant to the Workers' Compensation Law, must treat injuries pursuant to the relevant Medical Treatment Guidelines. The Medical Treatment Guidelines are posted on the Board's website. For additional information, please call (800) 781-2362.
12.The Medical Treatment Guidelines are the standard of care for injured workers.
13.HIPAA NOTICE - In order to adjudicate a workers' compensation claim, WCL § 13-a(4)(a) and 12 NYCRR § 325-1.3 require health care providers to regularly file medical reports of treatment with the Board and the insurer or employer. Pursuant to 45 CFR § 164.512 these legally required medical reports are exempt from HIPAA's restrictions on disclosure of health information.