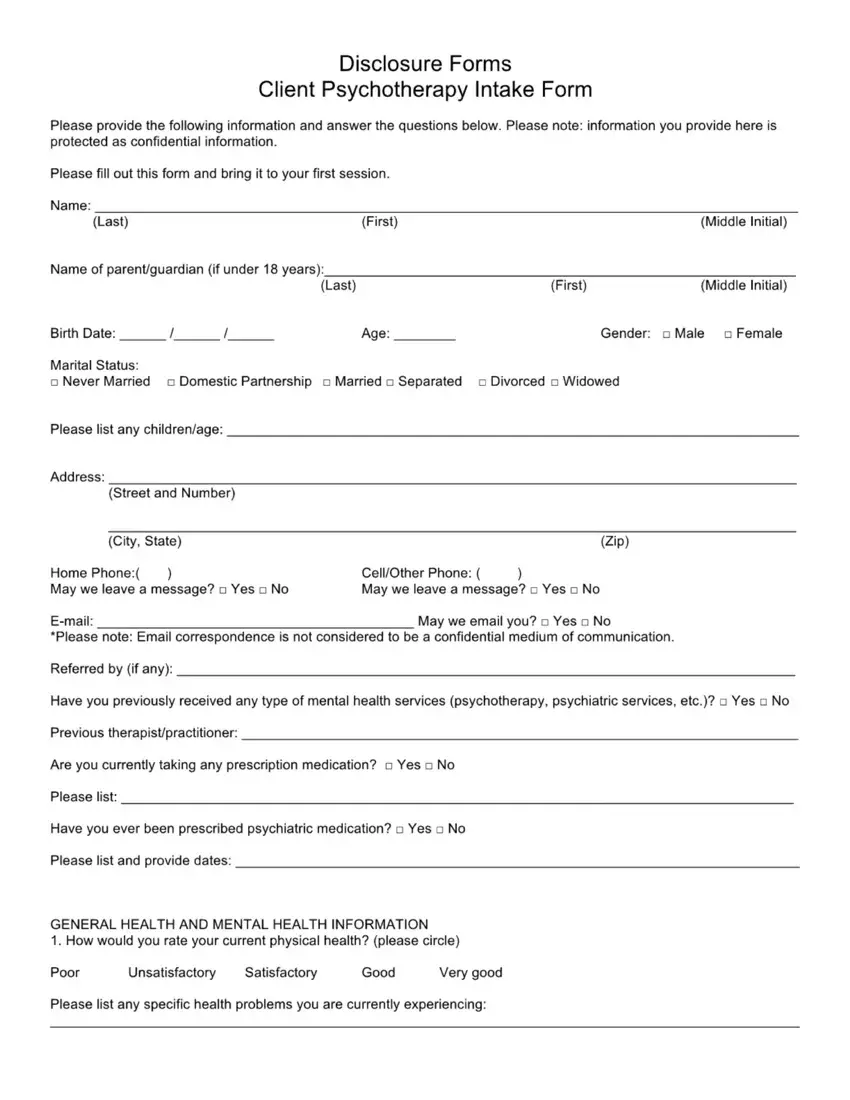
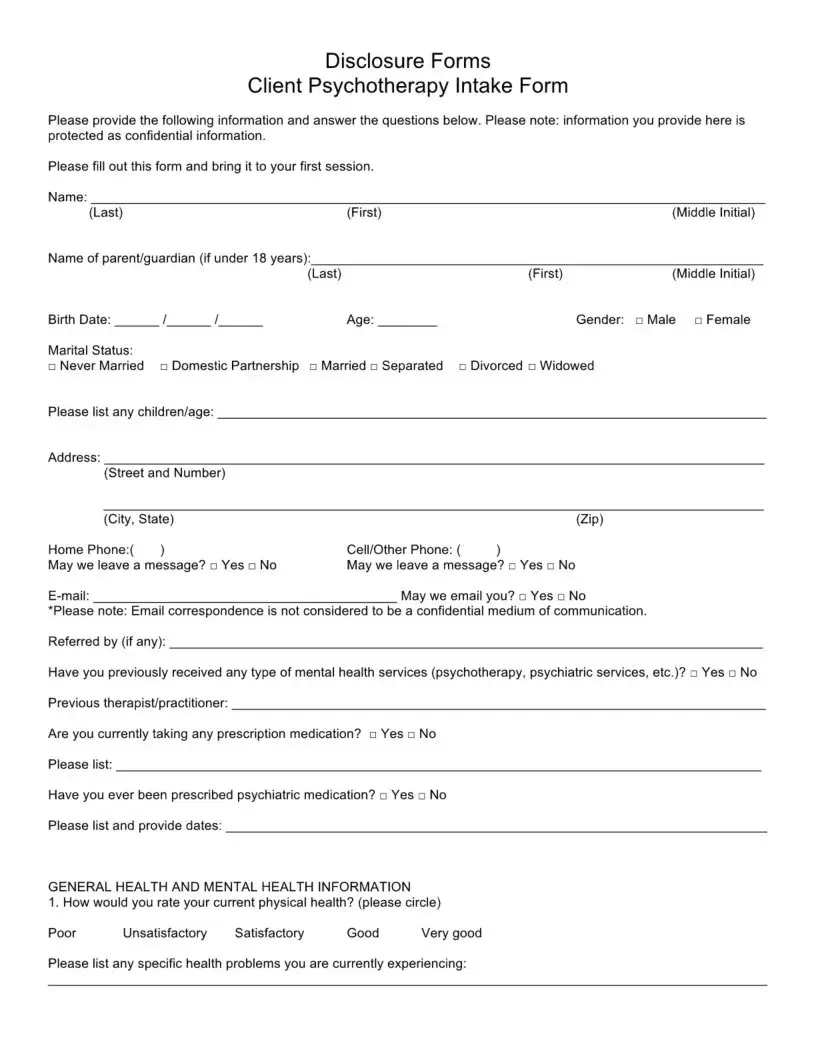
Disclosure Forms
Client Psychotherapy Intake Form
Please provide the following information and answer the questions below. Please note: information you provide here is protected as confidential information.
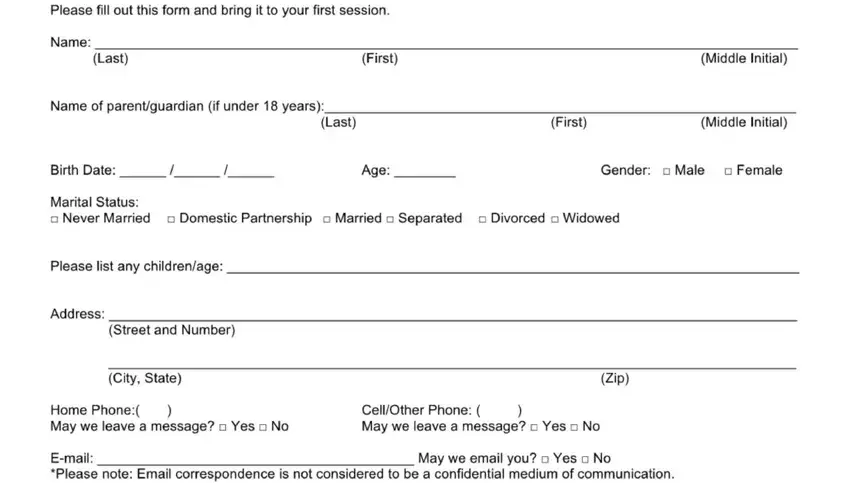
Please fill out this form and bring it to your first session.
Name: |
|
|
(Last) |
(First) |
(Middle Initial) |
Name of parent/guardian (if under 18 years):
|
|
|
(Last) |
(First) |
(Middle Initial) |
Birth Date: |
/ |
/ |
Age: |
Gender: |
□ Male □ Female |
Marital Status:
□Never Married □ Domestic Partnership □ Married □ Separated □ Divorced □ Widowed
Please list any children/age:
Address:
(Street and Number) |
|
|
(City, State) |
|
(Zip) |
Home Phone:( |
) |
Cell/Other Phone: ( |
) |
May we leave a message? □ Yes □ No |
May we leave a message? □ Yes □ No |
E-mail: |
|
May we email you? □ Yes □ No |
*Please note: Email correspondence is not considered to be a confidential medium of communication.
Referred by (if any):
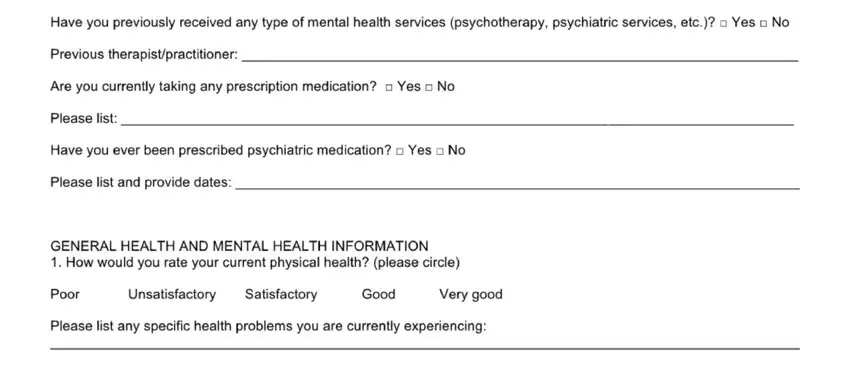
Have you previously received any type of mental health services (psychotherapy, psychiatric services, etc.)? □ Yes □ No
Previous therapist/practitioner:
Are you currently taking any prescription medication? □ Yes □ No
Please list:
Have you ever been prescribed psychiatric medication? □ Yes □ No
Please list and provide dates:
GENERAL HEALTH AND MENTAL HEALTH INFORMATION
1. How would you rate your current physical health? (please circle)
Poor |
Unsatisfactory |
Satisfactory |
Good |
Very good |
Please list any specific health problems you are currently experiencing:
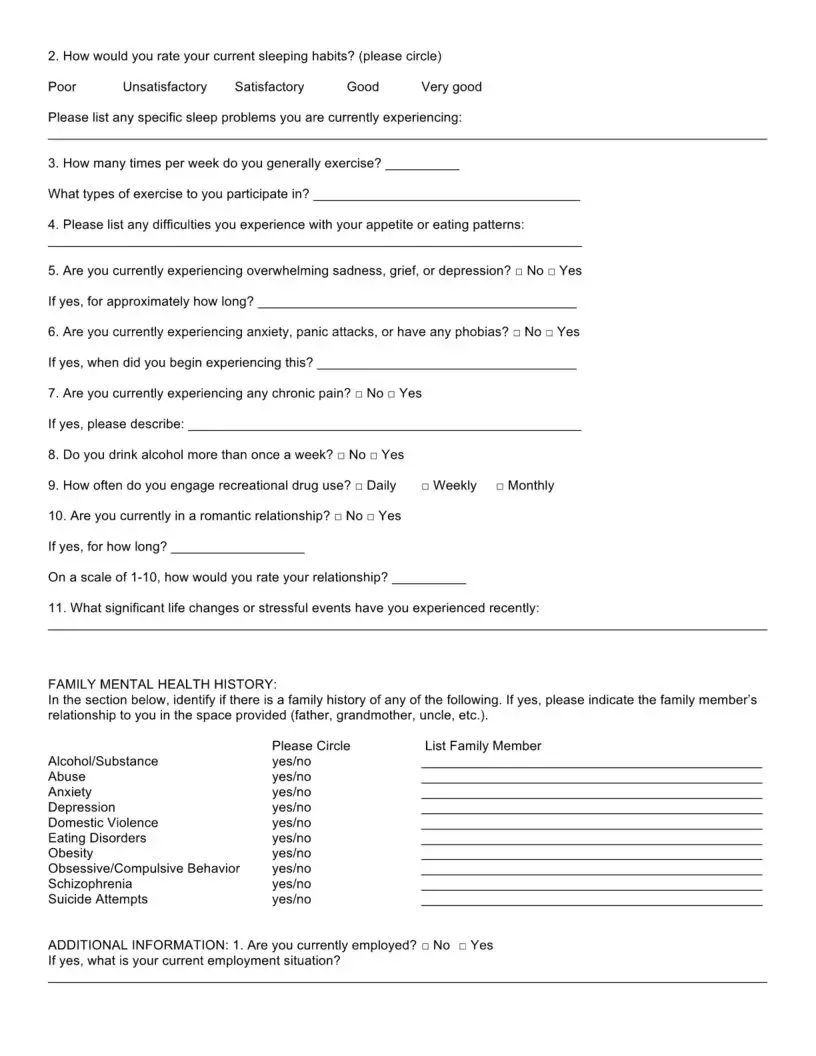
2. How would you rate your current sleeping habits? (please circle)
Poor |
Unsatisfactory |
Satisfactory |
Good |
Very good |
Please list any specific sleep problems you are currently experiencing:
3.How many times per week do you generally exercise? What types of exercise to you participate in?
4.Please list any difficulties you experience with your appetite or eating patterns:
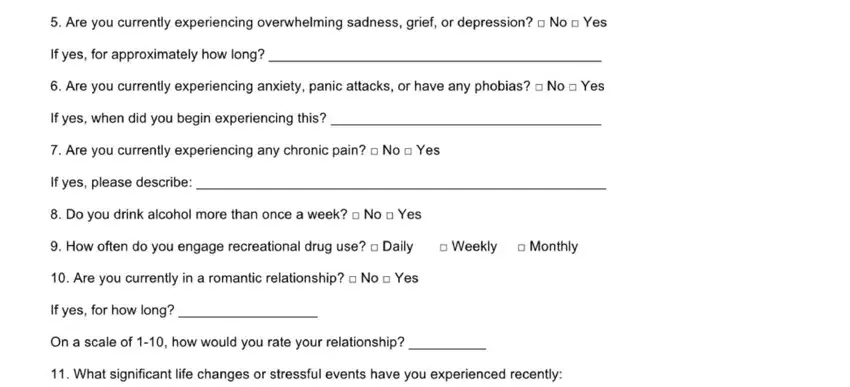
5.Are you currently experiencing overwhelming sadness, grief, or depression? □ No □ Yes If yes, for approximately how long?
6.Are you currently experiencing anxiety, panic attacks, or have any phobias? □ No □ Yes If yes, when did you begin experiencing this?
7.Are you currently experiencing any chronic pain? □ No □ Yes
If yes, please describe:
8. Do you drink alcohol more than once a week? □ No □ Yes
9. How often do you engage recreational drug use? □ Daily |
Weekly |
Monthly |
10.Are you currently in a romantic relationship? □ No □ Yes If yes, for how long?
On a scale of 1-10, how would you rate your relationship?
11.What significant life changes or stressful events have you experienced recently:
FAMILY MENTAL HEALTH HISTORY:
In the section below, identify if there isPlea familyse Circlehistory of any of theListfollowingFamily Member. If yes, please indicate the family member’s Alcohol/Substancerelationship to you in the space providedyes/no(father, grandmother, uncle, etc.).
Abuse |
yes/no |
Anxiety |
yes/no |
Depression |
yes/no |
Domestic Violence |
yes/no |
Eating Disorders |
yes/no |
Obesity |
yes/no |
Obsessive/Compulsive Behavior |
yes/no |
Schizophrenia |
yes/no |
Suicide Attempts |
yes/no |
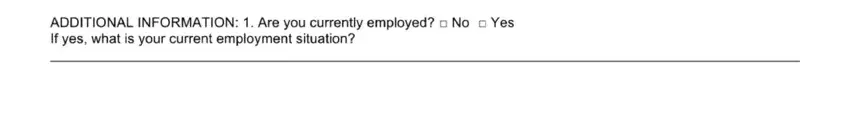
ADDITIONAL INFORMATION: 1. Are you currently employed? □ No □ Yes
If yes, what is your current employment situation?
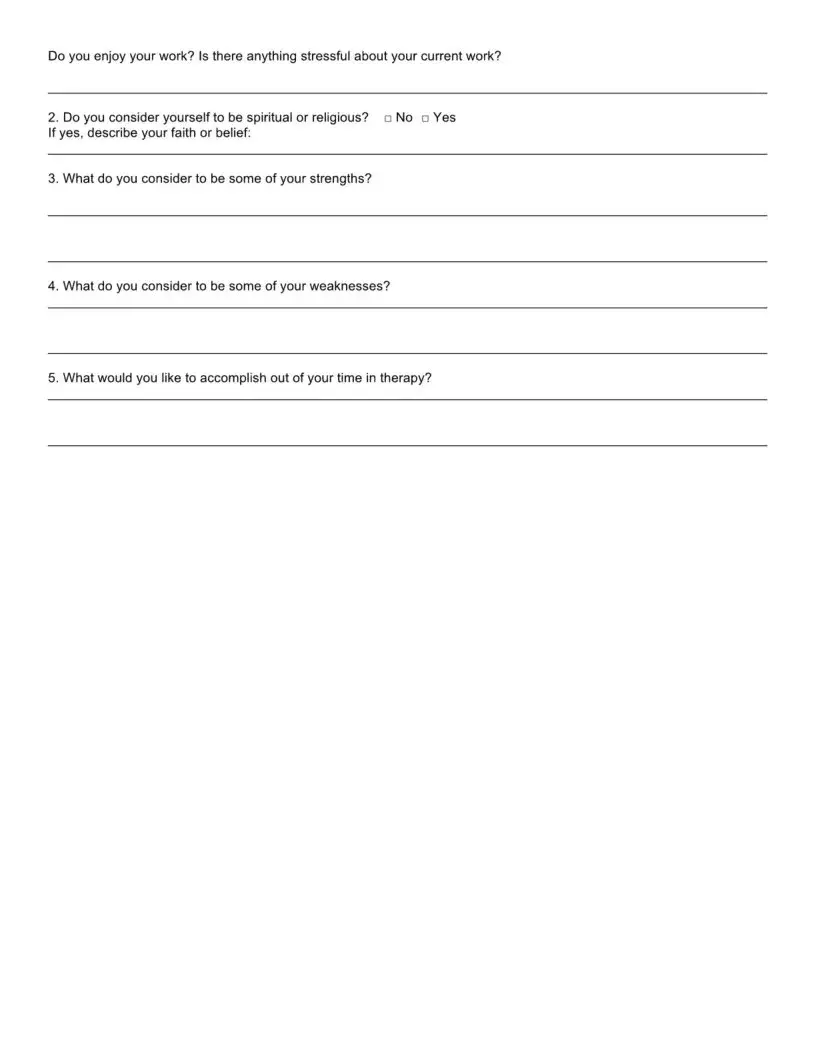
Do you enjoy your work? Is there anything stressful about your current work?
2. Do you consider yourself to be spiritual or religious? |
No Yes |
If yes, describe your faith or belief: |
|
3. What do you consider to be some of your strengths?
4.What do you consider to be some of your weaknesses?
5.What would you like to accomplish out of your time in therapy?
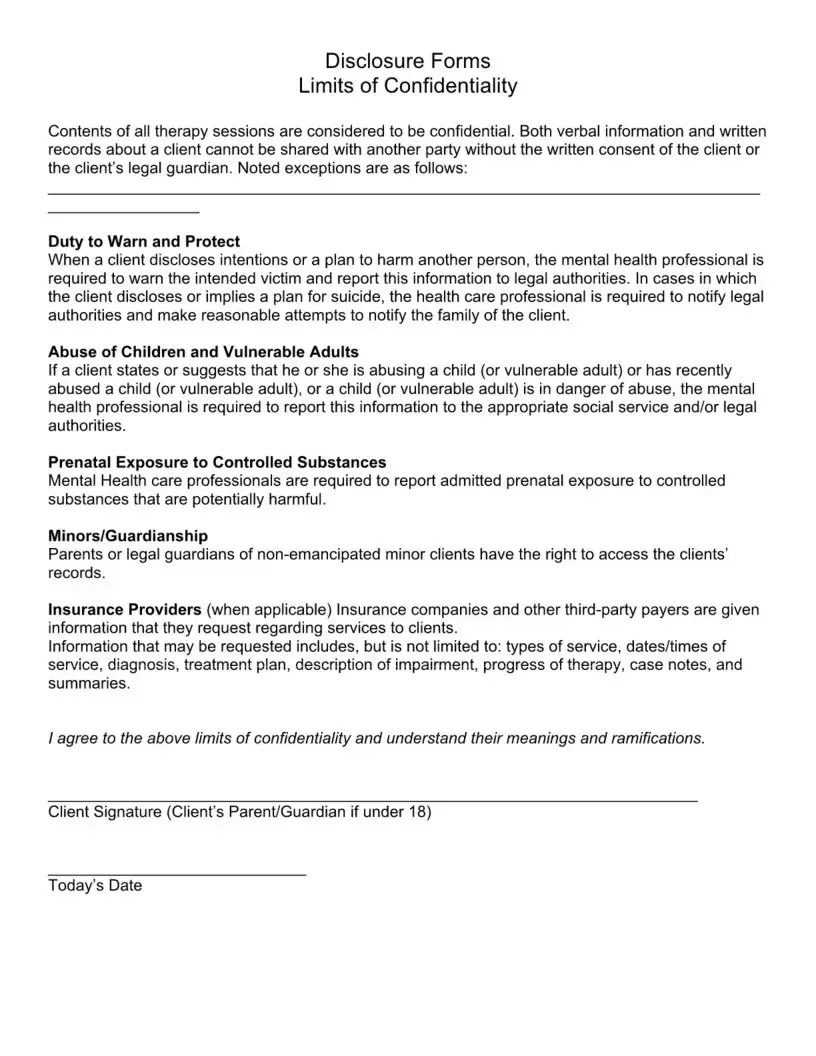
Disclosure Forms
Limits of Confidentiality
Contents of all therapy sessions are considered to be confidential. Both verbal information and written records about a client cannot be shared with another party without the written consent of the client or the client’s legal guardian. Noted exceptions are as follows:
Duty to Warn and Protect
When a client discloses intentions or a plan to harm another person, the mental health professional is required to warn the intended victim and report this information to legal authorities. In cases in which the client discloses or implies a plan for suicide, the health care professional is required to notify legal authorities and make reasonable attempts to notify the family of the client.
Abuse of Children and Vulnerable Adults
If a client states or suggests that he or she is abusing a child (or vulnerable adult) or has recently abused a child (or vulnerable adult), or a child (or vulnerable adult) is in danger of abuse, the mental health professional is required to report this information to the appropriate social service and/or legal authorities.
Prenatal Exposure to Controlled Substances
Mental Health care professionals are required to report admitted prenatal exposure to controlled substances that are potentially harmful.
Minors/Guardianship
Parents or legal guardians of non-emancipated minor clients have the right to access the clients’ records.
Insurance Providers (when applicable) Insurance companies and other third-party payers are given information that they request regarding services to clients.
Information that may be requested includes, but is not limited to: types of service, dates/times of service, diagnosis, treatment plan, description of impairment, progress of therapy, case notes, and summaries.
I agree to the above limits of confidentiality and understand their meanings and ramifications.
Client Signature (Client’s Parent/Guardian if under 18)
Disclosure Forms
Cancellation Policy
If you fail to cancel a scheduled appointment, we cannot use this time for another client and you will be billed for the entire cost of your missed appointment. A full session fee is charged for missed appointments or cancellations with less than a 24-hour notice unless it is due to illness or an emergency. A bill will be mailed directly to all clients who do not show up for, or cancel an appointment.
Thank you for your consideration regarding this important matter.
Client Signature (Client’s Parent/Guardian if under 18)
Today’s Date
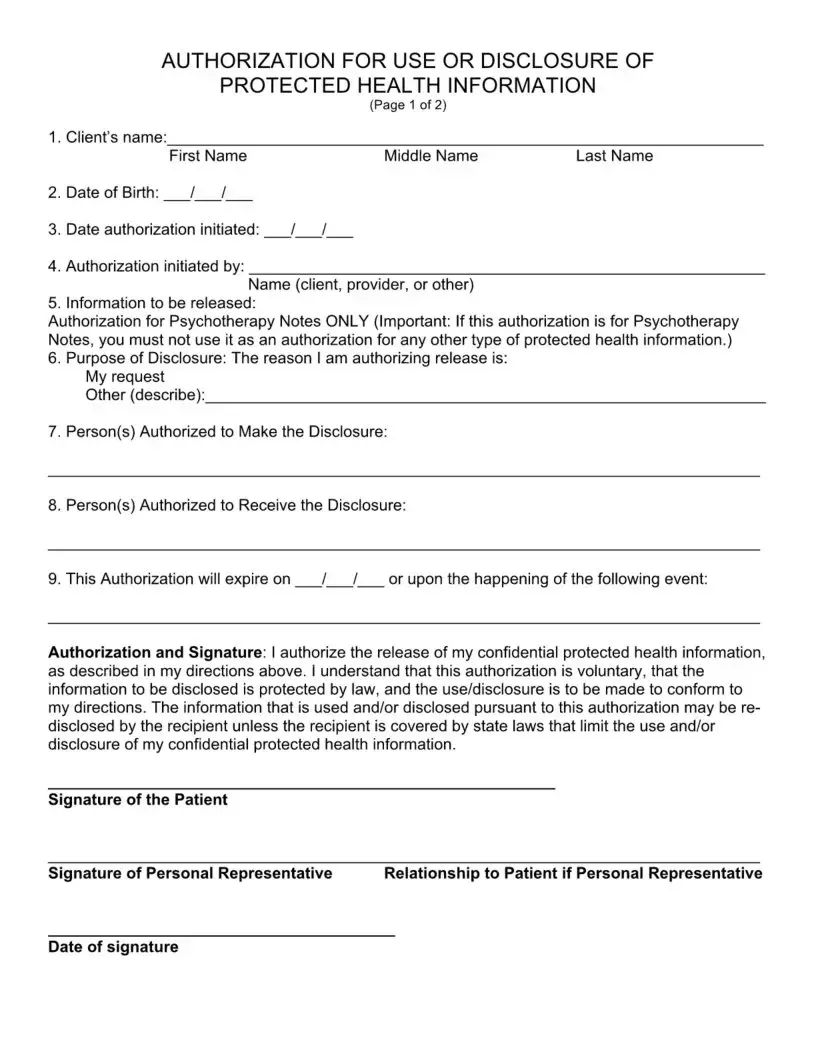
AUTHORIZATION FOR USE OR DISCLOSURE OF
PROTECTED HEALTH INFORMATION
(Page 1 of 2)
1. Client’s name:
First Name |
Middle Name |
Last Name |
2.Date of Birth: / /
3.Date authorization initiated: / /
4.Authorization initiated by:
Name (client, provider, or other)
5. Information to be released:
Authorization for Psychotherapy Notes ONLY (Important: If this authorization is for Psychotherapy Notes, you must not use it as an authorization for any other type of protected health information.)
6.Purpose of Disclosure: The reason I am authorizing release is: My request
Other (describe):
7.Person(s) Authorized to Make the Disclosure:
8.Person(s) Authorized to Receive the Disclosure:
9. This Authorization will expire on |
/ / |
or upon the happening of the following event: |
Authorization and Signature: I authorize the release of my confidential protected health information,
as described in my directions above. I understand that this authorization is voluntary, that the information to be disclosed is protected by law, and the use/disclosure is to be made to conform to my directions. The information that is used and/or disclosed pursuant to this authorization may be re disclosed by the recipient unless the recipient is covered by state laws that limit the use and/or disclosure of my confidential protected health information.
Signature of the Patient
Signature of Personal Representative Relationship to Patient if Personal Representative
PATIENT RIGHTS AND HIPAA AUTHORIZATIONS
(Page 2 of 2)
The following specifies your rights about this authorization under the Health Insurance Portability and Accountability Act of 1996, as amended from time to time (“HIPAA").
1.Tell your mental health professional if you don’t understand this authorization, and they will explain it to you.
2.You have the right to revoke or cancel this authorization at any time, except: (a) to the extent information has already been shared based on this authorization; or (b) this authorization was obtained as a condition of obtaining insurance coverage. To revoke or cancel this authorization, you must submit your request in writing to your mental health professional and your insurance company, if applicable.
3.You may refuse to sign this authorization. Your refusal to sign will not affect your ability to obtain treatment, make payment, or affect your eligibility for benefits. If you refuse to sign this authorization, and you are in a research-related treatment program, or have authorized your provider to disclose information about you to a third party, your provider has the right to decide not to treat you or accept you as a client in their practice.
4.Once the information about you leaves this office according to the terms of this authorization, this office has no control over how it will be used by the recipient. You need to be aware that at that point your information may no longer be protected by HIPAA.
5.If this office initiated this authorization, you must receive a copy of the signed authorization.
6.Special Instructions for completing this authorization for the use and disclosure of Psychotherapy Notes. HIPAA provides special protections to certain medical records known as "Psychotherapy Notes.” All Psychotherapy Notes recorded on any medium (i.e., paper, electronic) by a mental health professional (such as a psychologist or psychiatrist) must be kept by the author and filed separate from the rest of the client’s medical records to maintain a higher standard of protection. “Psychotherapy Notes” are defined under HIPAA as notes recorded by a health care provider who is a mental health professional documenting or analyzing the contents of conversation during a private counseling session or a group, joint, or family counseling session and that are separate from the rest of the individual’s medical records. Excluded from the “Psychotherapy Notes” definition are the following: (a) medication prescription and monitoring, (b) counseling session start and stop times, (c) the modalities and frequencies of treatment furnished, (d) the results of clinical tests, and (e) any summary of: diagnosis, functional status, the treatment plan, symptoms, prognosis, and progress to date.
In order for a medical provider to release “Psychotherapy Notes” to a third party, the client who is the subject of the Psychotherapy Notes must sign this authorization to specifically allow for the release of Psychotherapy Notes. Such authorization must be separate from an authorization to release other medical records.