Submitting documents together with our PDF editor is easier than nearly anything. To change prior auth request form superior the form, there is nothing you will do - just follow the actions down below:
Step 1: The initial step should be to select the orange "Get Form Now" button.
Step 2: You're now allowed to modify prior auth request form superior. You have a variety of options thanks to our multifunctional toolbar - you can add, erase, or modify the content, highlight its selected areas, as well as carry out many other commands.
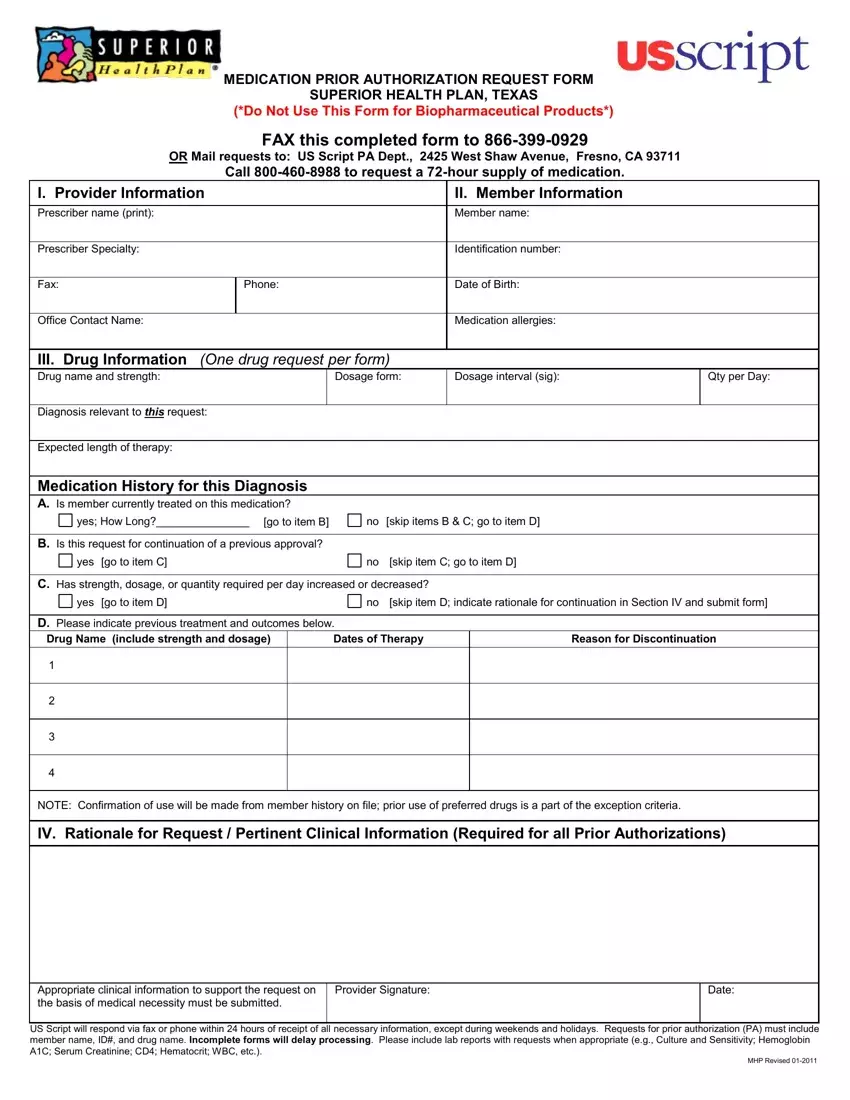
For you to obtain the document, type in the information the software will ask you to for each of the following sections:
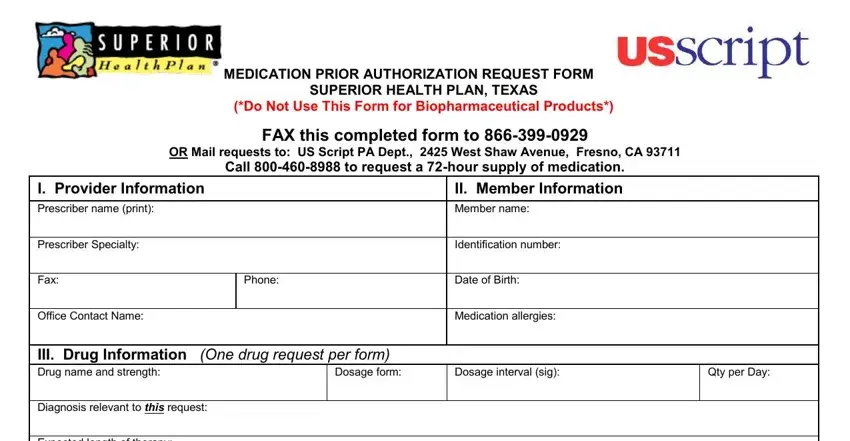
The program will require you to complete the Expected length of therapy, Medication History for this, yes How Long, go to item B, no skip items B C go to item D, B Is this request for continuation, yes go to item C, no skip item C go to item D, C Has strength dosage or quantity, yes go to item D, no skip item D indicate rationale, D Please indicate previous, Drug Name include strength and, Dates of Therapy, and Reason for Discontinuation segment.
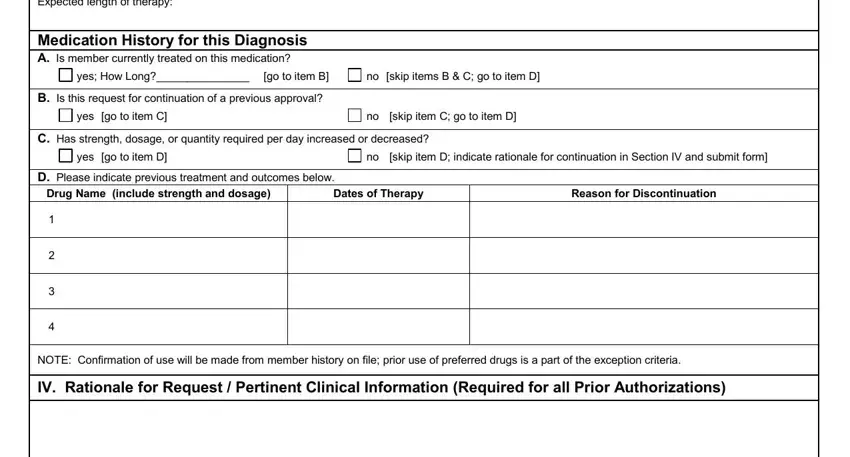
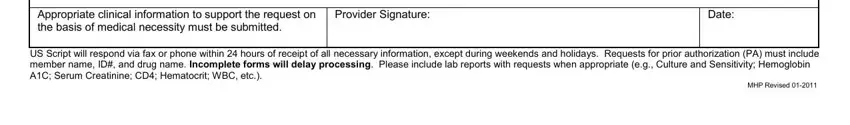
You'll be requested for some important details if you need to fill up the Appropriate clinical information, Provider Signature, Date, US Script will respond via fax or, and MHP Revised box.
Step 3: Hit the Done button to save your document. Now it is at your disposal for transfer to your device.
Step 4: Prepare copies of the file. This will protect you from upcoming misunderstandings. We don't look at or disclose your information, therefore feel comfortable knowing it will be protected.