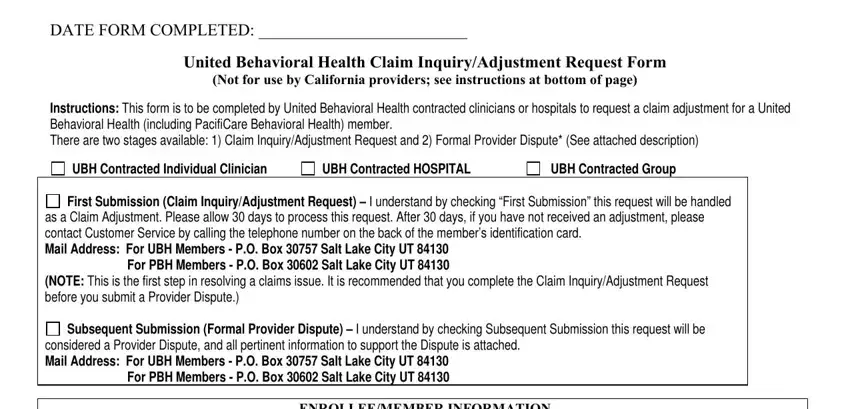
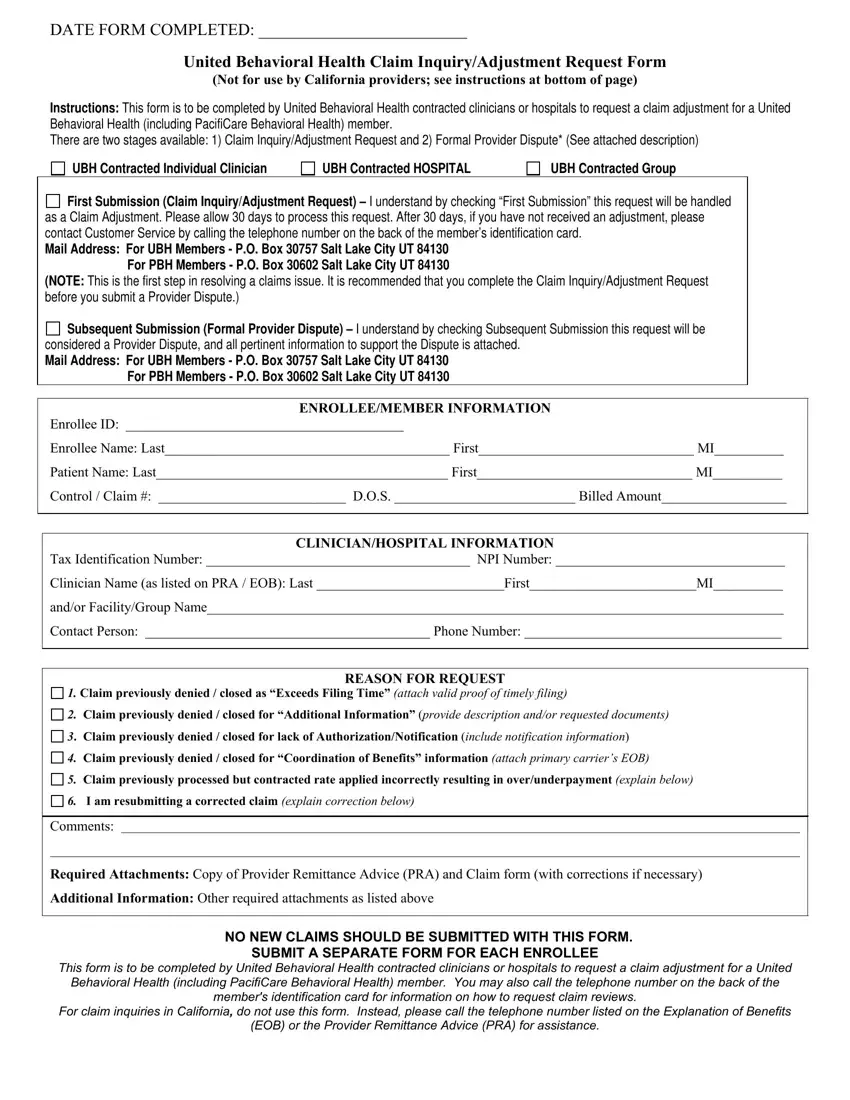
First Submission (Claim Inquiry/Adjustment Request) – I understand by checking “First Submission” this request will be handled as a Claim Adjustment. Please allow 30 days to process this request. After 30 days, if you have not received an adjustment, please contact Customer Service by calling the telephone number on the back of the member’s identification card.
First Submission (Claim Inquiry/Adjustment Request) – I understand by checking “First Submission” this request will be handled as a Claim Adjustment. Please allow 30 days to process this request. After 30 days, if you have not received an adjustment, please contact Customer Service by calling the telephone number on the back of the member’s identification card.
Mail Address: For UBH Members - P.O. Box 30757 Salt Lake City UT 84130
For PBH Members - P.O. Box 30602 Salt Lake City UT 84130
(NOTE: This is the first step in resolving a claims issue. It is recommended that you complete the Claim Inquiry/Adjustment Request before you submit a Provider Dispute.)

 Subsequent Submission (Formal Provider Dispute) – I understand by checking Subsequent Submission this request will be considered a Provider Dispute, and all pertinent information to support the Dispute is attached.
Subsequent Submission (Formal Provider Dispute) – I understand by checking Subsequent Submission this request will be considered a Provider Dispute, and all pertinent information to support the Dispute is attached.
Mail Address: For UBH Members - P.O. Box 30757 Salt Lake City UT 84130
For PBH Members - P.O. Box 30602 Salt Lake City UT 84130
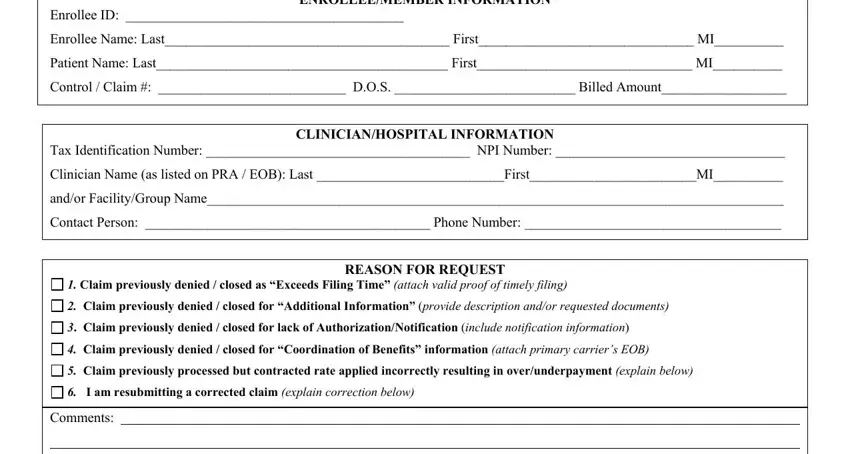
ENROLLEE/MEMBER INFORMATION
Enrollee ID: ________________________________________
Enrollee Name: Last_________________________________________ First_______________________________ MI__________
Patient Name: Last__________________________________________ First_______________________________ MI__________
Control / Claim #: ___________________________ D.O.S. __________________________ Billed Amount__________________
CLINICIAN/HOSPITAL INFORMATION
Tax Identification Number: ______________________________________ NPI Number: _________________________________
Clinician Name (as listed on PRA / EOB): Last ___________________________First________________________MI__________
and/or Facility/Group Name___________________________________________________________________________________
Contact Person: _________________________________________ Phone Number: _____________________________________
REASON FOR REQUEST
1. Claim previously denied / closed as “Exceeds Filing Time” (attach valid proof of timely filing)
2. Claim previously denied / closed for “Additional Information” (provide description and/or requested documents)
3. Claim previously denied / closed for lack of Authorization/Notification (include notification information)
4. Claim previously denied / closed for “Coordination of Benefits” information (attach primary carrier’s EOB)
5. Claim previously processed but contracted rate applied incorrectly resulting in over/underpayment (explain below)
6. I am resubmitting a corrected claim (explain correction below)
Comments:
Required Attachments: Copy of Provider Remittance Advice (PRA) and Claim form (with corrections if necessary)
Additional Information: Other required attachments as listed above
NO NEW CLAIMS SHOULD BE SUBMITTED WITH THIS FORM.
SUBMIT A SEPARATE FORM FOR EACH ENROLLEE
This form is to be completed by United Behavioral Health contracted clinicians or hospitals to request a claim adjustment for a United Behavioral Health (including PacifiCare Behavioral Health) member. You may also call the telephone number on the back of the member's identification card for information on how to request claim reviews.
For claim inquiries in California, do not use this form. Instead, please call the telephone number listed on the Explanation of Benefits
(EOB) or the Provider Remittance Advice (PRA) for assistance.