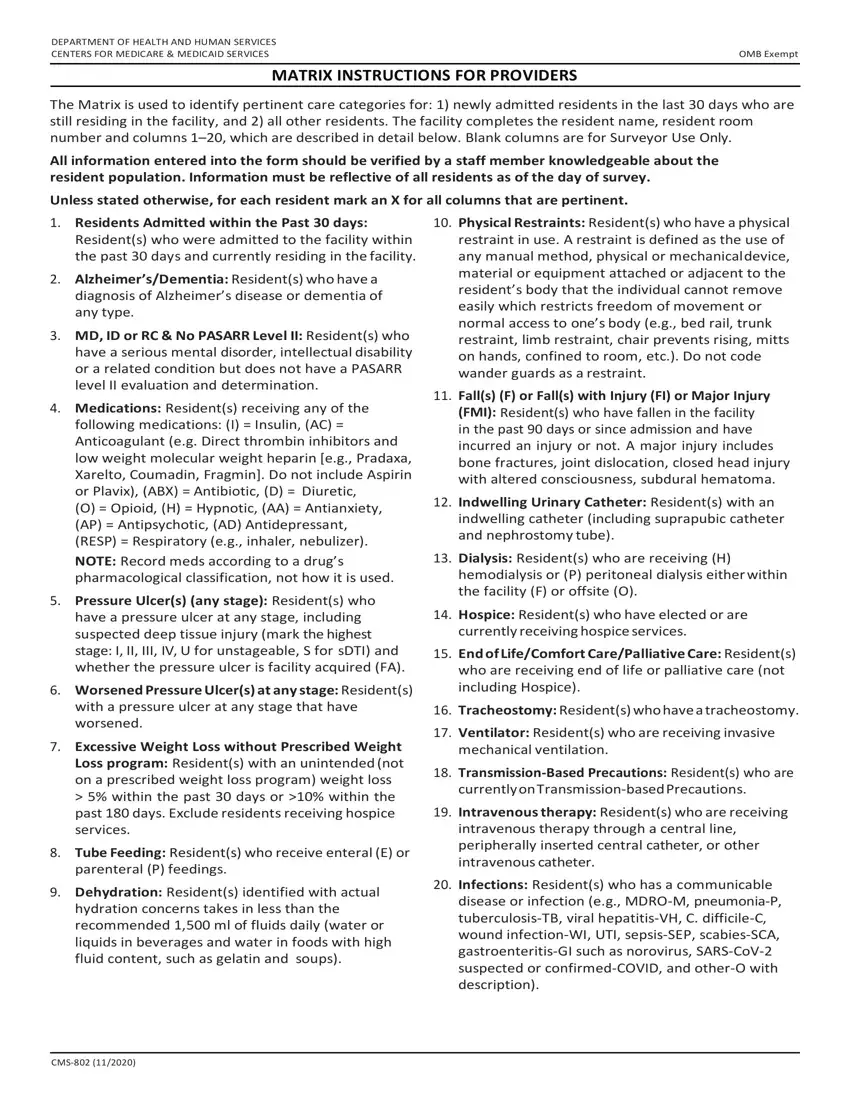
1.Residents Admitted within the Past 30 days: Resident(s) who were admitted to the facility within the past 30 days and currently residing in the facility.
2.Alzheimer’s/Dementia: Resident(s) who have a diagnosis of Alzheimer’s disease or dementia of any type.
3.MD, ID or RC & No PASARR Level II: Resident(s) who have a serious mental disorder, intellectual disability or a related condition but does not have a PASARR level II evaluation and determination.
4.Medications: Resident(s) receiving any of the
following medications: (I) = Insulin, (AC) = Anticoagulant (e.g. Direct thrombin inhibitors and low weight molecular weight heparin [e.g., Pradaxa, Xarelto, Coumadin, Fragmin]. Do not include Aspirin or Plavix), (ABX) = Antibiotic, (D) = Diuretic,
(O) = Opioid, (H) = Hypnotic, (AA) = Antianxiety, (AP) = Antipsychotic, (AD) Antidepressant, (RESP) = Respiratory (e.g., inhaler, nebulizer).
NOTE: Record meds according to a drug’s pharmacological classification, not how it is used.
5.Pressure Ulcer(s) (any stage): Resident(s) who have a pressure ulcer at any stage, including suspected deep tissue injury (mark the highest stage: I, II, III, IV, U for unstageable, S for sDTI) and whether the pressure ulcer is facility acquired (FA).
6.Worsened Pressure Ulcer(s) at any stage: Resident(s) with a pressure ulcer at any stage that have worsened.
7.Excessive Weight Loss without Prescribed Weight Loss program: Resident(s) with an unintended (not on a prescribed weight loss program) weight loss > 5% within the past 30 days or >10% within the past 180 days. Exclude residents receiving hospice services.
8.Tube Feeding: Resident(s) who receive enteral (E) or parenteral (P) feedings.
9.Dehydration: Resident(s) identified with actual hydration concerns takes in less than the recommended 1,500 ml of fluids daily (water or liquids in beverages and water in foods with high fluid content, such as gelatin and soups).
10.Physical Restraints: Resident(s) who have a physical restraint in use. A restraint is defined as the use of any manual method, physical or mechanicaldevice, material or equipment attached or adjacent to the resident’s body that the individual cannot remove easily which restricts freedom of movement or normal access to one’s body (e.g., bed rail, trunk restraint, limb restraint, chair prevents rising, mitts on hands, confined to room, etc.). Do not code wander guards as a restraint.
11.Fall(s) (F) or Fall(s) with Injury (FI) or Major Injury (FMI): Resident(s) who have fallen in the facility in the past 90 days or since admission and have incurred an injury or not. A major injury includes bone fractures, joint dislocation, closed head injury with altered consciousness, subdural hematoma.
12.Indwelling Urinary Catheter: Resident(s) with an indwelling catheter (including suprapubic catheter and nephrostomy tube).
13.Dialysis: Resident(s) who are receiving (H) hemodialysis or (P) peritoneal dialysis either within the facility (F) or offsite (O).
14.Hospice: Resident(s) who have elected or are currently receiving hospice services.
15.End of Life/Comfort Care/Palliative Care: Resident(s) who are receiving end of life or palliative care (not including Hospice).
16.Tracheostomy: Resident(s) who have a tracheostomy.
17.Ventilator: Resident(s) who are receiving invasive mechanical ventilation.
18.Transmission-Based Precautions: Resident(s) who are currently onTransmission-basedPrecautions.
19.Intravenous therapy: Resident(s) who are receiving intravenous therapy through a central line, peripherally inserted central catheter, or other intravenous catheter.
20.Infections: Resident(s) who has a communicable disease or infection (e.g., MDRO-M, pneumonia-P, tuberculosis-TB, viral hepatitis-VH, C. difficile-C, wound infection-WI, UTI, sepsis-SEP, scabies-SCA, gastroenteritis-GI such as norovirus, SARS-CoV-2 suspected or confirmed-COVID, and other-O with description).
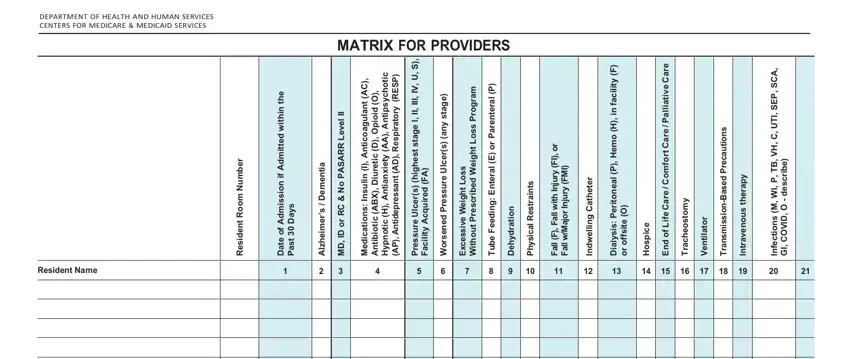


















 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21
2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21