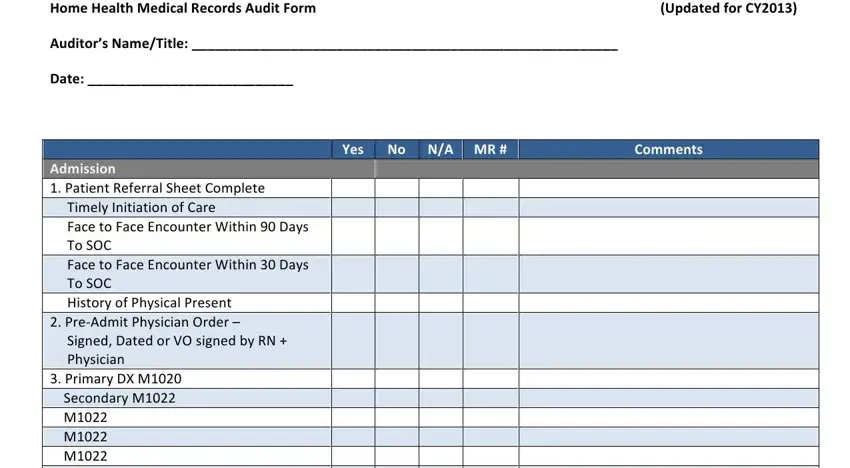
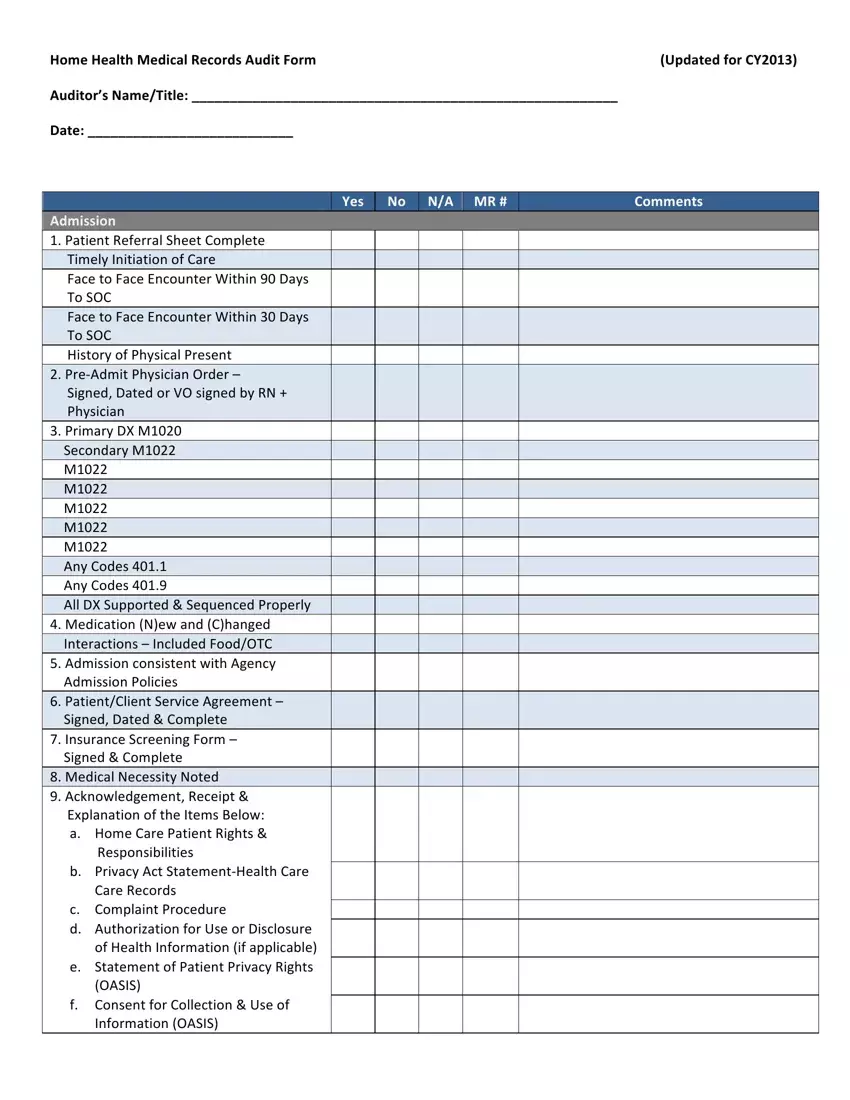
Home Health Medical Records Audit Form |
(Updated for CY2013) |
Auditor’s Name/Title: ________________________________________________________ |
|
Date: ___________________________ |
|
Admission
1.Patient Referral Sheet Complete Timely Initiation of Care
Face to Face Encounter Within 90 Days To SOC
Face to Face Encounter Within 30 Days To SOC
History of Physical Present
2.Pre‐Admit Physician Order –
Signed, Dated or VO signed by RN + Physician
3.Primary DX M1020 Secondary M1022 M1022
M1022
M1022
M1022
M1022
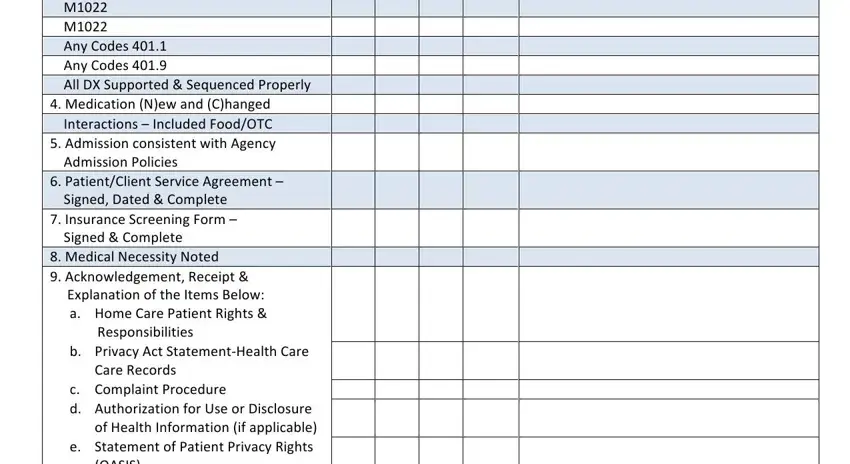
Any Codes 401.1 Any Codes 401.9
All DX Supported & Sequenced Properly
4.Medication (N)ew and (C)hanged Interactions – Included Food/OTC
5.Admission consistent with Agency Admission Policies
6.Patient/Client Service Agreement – Signed, Dated & Complete
7.Insurance Screening Form – Signed & Complete
8.Medical Necessity Noted
9.Acknowledgement, Receipt & Explanation of the Items Below:
a.Home Care Patient Rights & Responsibilities
b.Privacy Act Statement‐Health Care Care Records
c.Complaint Procedure
d.Authorization for Use or Disclosure of Health Information (if applicable)
e.Statement of Patient Privacy Rights (OASIS)
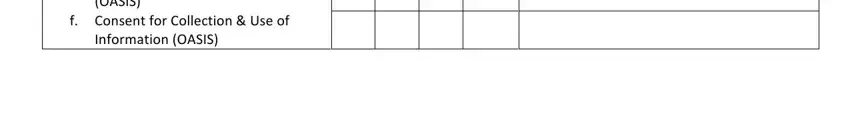
f.Consent for Collection & Use of Information (OASIS)
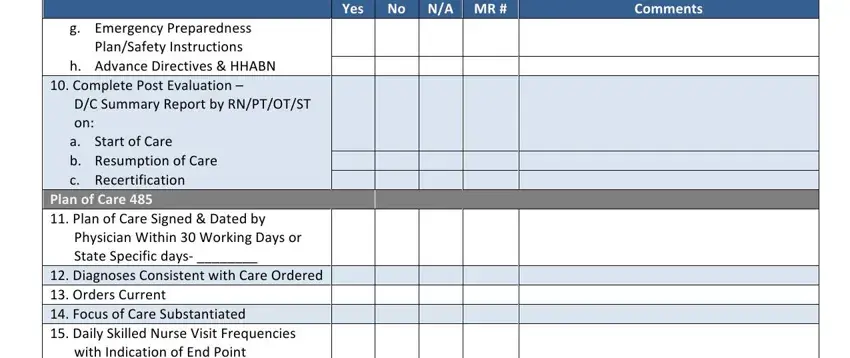
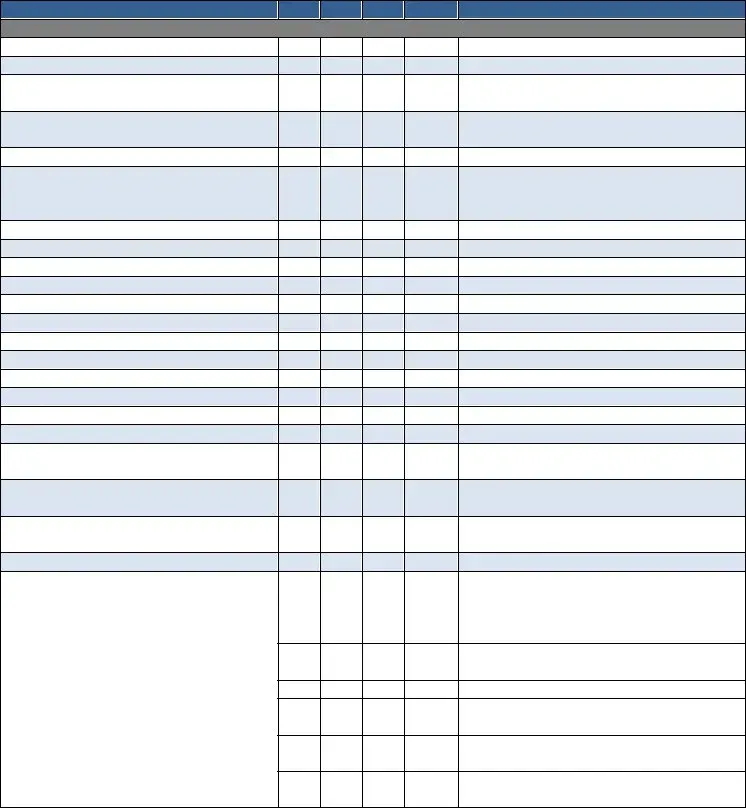
g.Emergency Preparedness Plan/Safety Instructions
h.Advance Directives & HHABN
10. Complete Post Evaluation –
D/C Summary Report by RN/PT/OT/ST on:
a. Start of Care
b. Resumption of Care
c. Recertification
Plan of Care 485
11.Plan of Care Signed & Dated by Physician Within 30 Working Days or State Specific days‐ ________
12.Diagnoses Consistent with Care Ordered
13.Orders Current
14. Focus of Care Substantiated
15.Daily Skilled Nurse Visit Frequencies with Indication of End Point
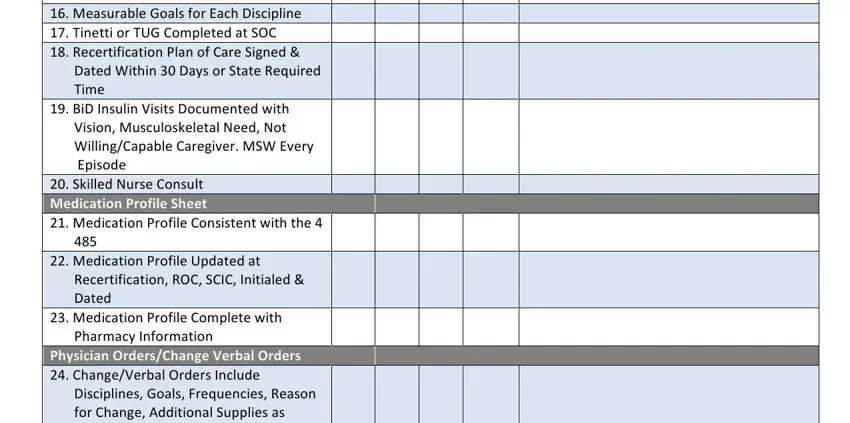
16. Measurable Goals for Each Discipline
17. Tinetti or TUG Completed at SOC
18. Recertification Plan of Care Signed &
Dated Within 30 Days or State Required
Time
19.BiD Insulin Visits Documented with Vision, Musculoskeletal Need, Not Willing/Capable Caregiver. MSW Every Episode
20. Skilled Nurse Consult
Medication Profile Sheet
21.Medication Profile Consistent with the 4 485
22. Medication Profile Updated at
Recertification, ROC, SCIC, Initialed &
Dated
23.Medication Profile Complete with Pharmacy Information
Physician Orders/Change Verbal Orders
24. Change/Verbal Orders Include Disciplines, Goals, Frequencies, Reason for Change, Additional Supplies as Appropriate
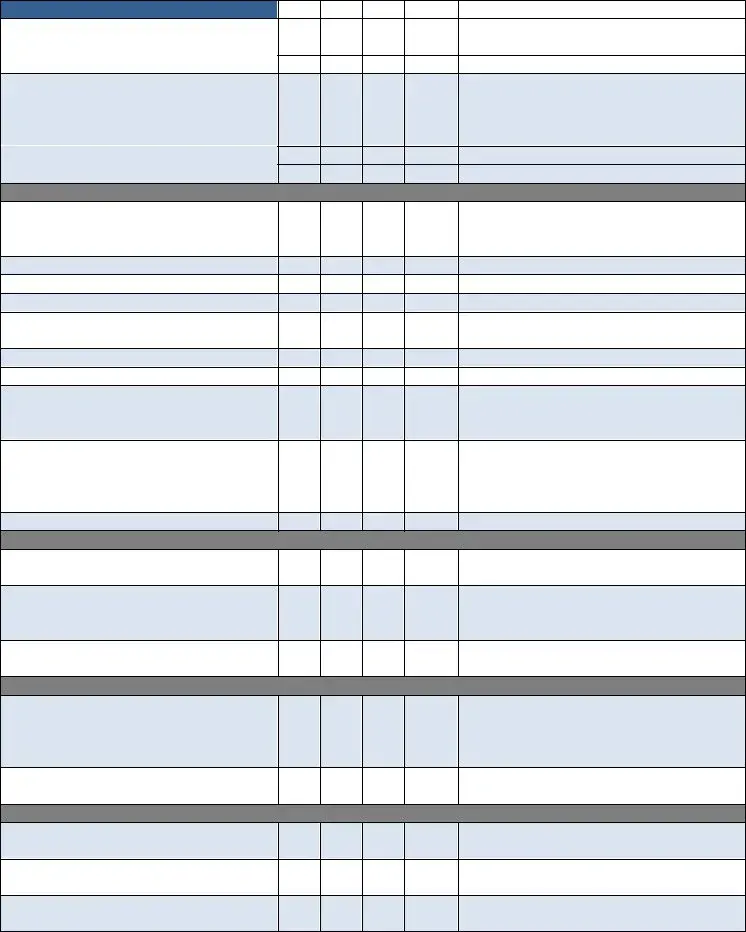
25.Change Orders Signed & Dated by Physician Within 30 Working Days
OASIS Assessment Form
26. Complete, Signed & Dated by:
___________________________
27.M2200 Answer Meets the Threshold for a Medicare High Case Mix Group
28. M1020 & M1022 Diagnoses & ICD‐9 are Consistent with the Plan of Care
29.All OASIS Assessments Were Exported Within 30 Days
30. OASIS Recertifications Were Done
Within 5 Days of the End of the Episode
31.All OASIS Were Reviewed for Consistency in Coordination with the Discipline Who Completed the Form
Skilled Nursing Clinical Notes
32. Visit Frequencies & Duration are Consistent with Physician Orders
33.Orders Written for Visit Frequencies/ Treatment Change
34. Homebound Status Supported on Each Visit Note
35.Measurable Goals for Each Discipline with Specific Time Frames
36. Frequency of Visits Appropriate for Patient’s Needs & Interventions Provided
37. Appropriate Missed Visit (MV) Notes
38. Skilled Care Evident on Each Note
39. Evidence of Coordination of Care
40. Every Note Signed & Dated
41. Follows the Plan of Care (485)
42. Weekly Wound Reports are Completed
43. Missed Visit Reports are Completed
44. Pain Assessment Done Every Visit with Intervention (If Applicable)
45.Abnormal Vital Signs Reported to Physician & Case Managers
46. Evidence of Interventions with Abnormal Parameters/Findings
47.Skilled Nurse Discharge Summary/ Instructions Completed
48. LVN Supervisory Visit Every 30 Days by Registered Nurse
Certified Home Health Aide
49.Visit Frequencies & Duration Consistent with Physician Orders
50. Personal Care Instructions Documented,
Signed & Dated
51.Personal Care Instructions Modified as Appropriate
52. Notes Consistent with Personal Care Instructions Noted on the CHHA Assignment Sheet Completed by the RN/PT/ST/OT
53.Notes Reflect Supervisor Notification of Patient Complications or Changes
54. Visit Frequencies Appropriate for Patient Needs
55. Each Note Reflects Personal Care Given
56. Supervisory Visits at Least Every 14 Days by RN or PT
57. Every Note Signed & Dated
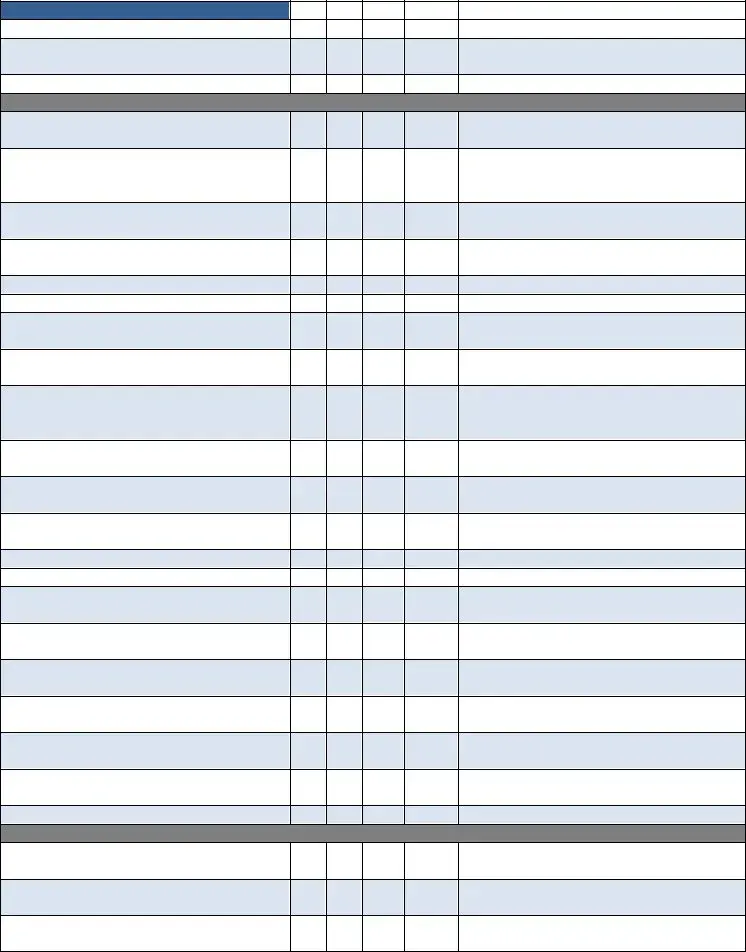
PT
58. Assessment Includes Evaluation,
Care Plan & Visit Note
59.Evaluation Done Within 48 Hours of Referral Physician Order or Date Ordered
60. Visit Frequencies/Duration Consistent with Physician Orders
61.Evidence of Need for Therapy/Social Service
62. Appropriate Missed Visit (MV) Notes
63. Notes Consistent with Physician Orders
64. Evidence of Skilled Service(s) Provided
in Each Note
65.Treatment/Services Provided Consistent with Physician Orders & Care Plan
66. Notes Reflect Supervisor & Physician Notification of Patient Complications or Changes
67.Specific Evaluation & “TREAT” Orders Prior to Care
68. Verbal Orders for “TREAT” Orders Prior to Care
69.Homebound Status Validated in Each Visit Note
70. Notes Reflect Progress Toward Goals
71. Evidence of Discharge Planning
72. Evidence of Therapy Home Exercise
Program
73.Discharge/Transfer Summary Complete with Goals Met/Unmet
74. Assessment & Evaluation performed by Qualified Therapist Every 30 Days
75.Supervision of PTA/OTA at Least Every 2 Weeks
76. Qualified Therapy Visit 13th Visit (11, 12, 13)
77.Qualified Therapy Visit 19th Visit (17, 18, 19)
78. Every Visit Note Signed & Dated
SLP
79.Assessment Includes Evaluation, Care Plan & Visit Note
80. Evaluation Done Within 48 Hours of Referral Physician Order or Date Ordered
81.Visit Frequencies/Duration Consistent with Physician Orders
82. Evidence of Need for Therapy/Social Service
83. Appropriate Missed Visit (MV) Note
84. Notes Consistent with Physician Orders
85.Evidence of Skilled Service(s) Provided in Each Note
86. Treatment/Services Provided Consistent with Physician Orders & Care Plan
87.Notes Reflect Supervisor & Physician Notification of Patient Complications or Changes
88. Homebound Status Validated in Each Visit
Note
89. Notes Reflect Progress Toward Goals
90. Evidence of Discharge Planning
91.Evidence of Therapy Home Exercise Program
92. Discharge/Transfer Summary Complete with Goals Met/Unmet
93.Supervision of PTA/OTA at Least Every 2 Weeks
94. Every Visit Note Signed & Dated
Miscellaneous
95.Progress Summary Completed(30‐45Days) Each Episode Signed & Dated
96. Field Notes are Submitted & Complete
97. Chart in Chronological Order
98. Chart in Order per Agency Policy
99.Patient Name & Medical Records Number on Every Page
100. Physician Orders are Completed/ Updated for Clinical Tests Such as:
a. Coumadin: Protime/INR
b. Hemoglobin A1C
c. CBC, Metabolic Panel, CMP
d. Others: _______________________
101.Communication with Physician Regarding Test Results
Process Measures:
Timely Initiation of Care
Influenza Received
PPV Ever Received
Heart Failure
DM Foot Care & Education
Pain Assessment
Pain Intervention
Depression Assessment
Medication Education
Falls Risk Assessment
Pressure Ulcer Prevention
Pressure Ulcer Risk Assessment
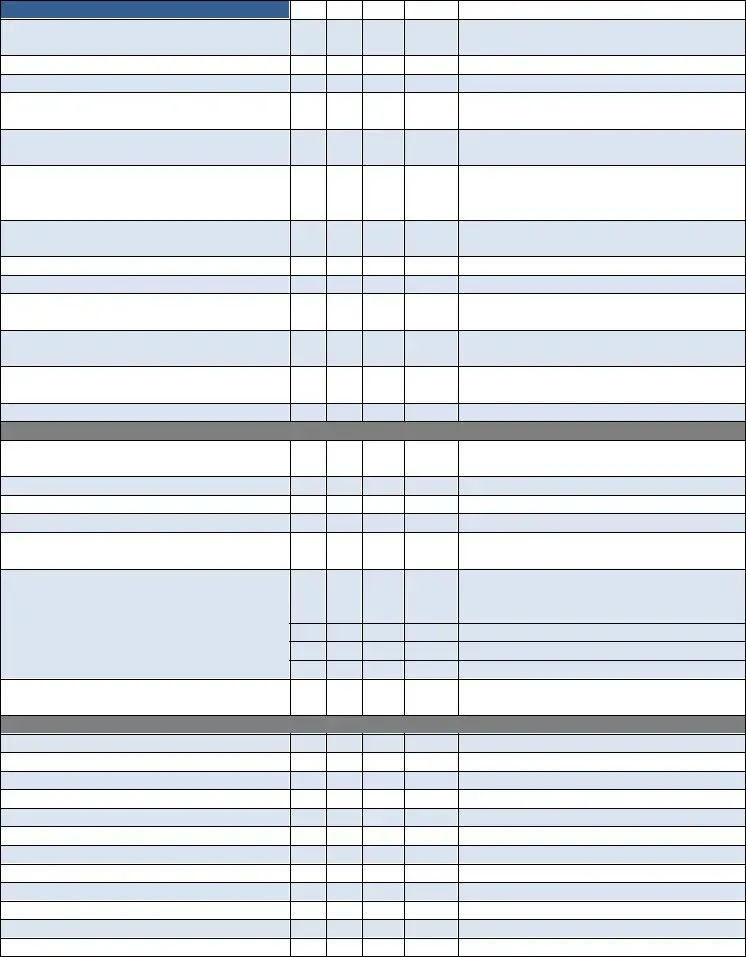
Additional Comments/Recommendations ‐
__________________________________________________________________________________________________
__________________________________________________________________________________________________
__________________________________________________________________________________________________
__________________________________________________________________________________________________
__________________________________________________________________________________________________
__________________________________________________________________________________________________
THE FOLLOWING IS APPLICABLE FOR QUARTERLY MEDICAL REVIEW REPORT
REVIEWED AND SIGNED BY THE FOLLOWING DISCIPLINARY REPRESENTATIVE
______________________________________ |
______________________________________ |
Registered Nurse |
Occupational Therapist (If Applicable) |
______________________________________ |
______________________________________ |
Physical Therapist (If Applicable) |
Speech Language Pathologist (If Applicable) |
______________________________________ |
______________________________________ |
Medical Director |
MSW (If Applicable) |
MR # ______________________