PROVIDER ACTION REQUEST FORM INSTRUCTIONS
Providers may request corrective adjustments to any previous payment, using the Provider Action Request (PAR) Form, and Medical Mutual® (Company) may make such adjustments as necessary and appropriate. Please note, however, that the Company has no obligation to make any adjustment after 12 months from the date the initial claim was processed.
Required Information
The PAR Form is used to help process provider inquiries in a more timely manner. All data fields must be completed. Forms not completed properly or provider inquiries not submitted with a form will be returned. Original submissions should have only one inquiry per form. Use a separate PAR Form for each patient.
Provider Information
Fill in the defined fields: the provider and tax identification number; contact person and telephone number; and the mailing address, including zip code. Provide e-mail address when available.
Patient Information
All patient data must be given. Always list the Company claim number as well as dates of service.
Type of Request
The PAR Form is used for all provider inquiries and provider appeals related to reimbursement. Check one Type of Request that best describes your request.
Care Management: When questioning reimbursement due to medical necessity, claim copies are not needed unless the original claim form data is being changed as a part of the request. Medical records must be attached. The needed records have been grouped by services.
•Allergy: All office notes for the services in question and a description of all medications given, including dosage.
•Ambulance — emergency room reports: Air — flight records, including a breakdown of charges that identify the number of air miles and a letter of medical necessity that substantiates the need for transfer; the place or origin of flight; and the destination; Ground — the run report from the ambulance company.
•Anesthesia: Hospital anesthesia records and operative reports.
•Behavioral Health: Inpatient medical records. For the medical care cases, physician’s signed written progress notes for the services in question.
•Cardiology: Medical history and test results.
•Complex Surgery: When questioning the level of reimbursement due to performance of additional services or services with a high level of difficulty, claim copies are not needed if the modifiers appear on the original claim submittal. It you are adding a modifying reason, you must submit a new claim form. Operative reports are required for Modifier 22. Incidental procedure denials require operative reports and/or office notes.
Type of Request continued
Page 2
•Concurrent Medical Care: All physician’s signed progress notes for the date of service in question.
•Cosmetic: Operative notes and pre-op photos and clinical notes.
•Institutional Outpatient and Professional Dental: Entire medical records, including operative notes, procedure notes, anesthesia records and/or the physician’s office notes, and preoperative panorex x-rays.
For lesion removals, the pathology reports (required).
•Emergency Room: For faster resolution submit complete ER records via fax (877)321-6664 or mail to
Medical Mutual Care Management MZ01-5b-3982 2060 E. 9th Street Cleveland OH, 44114. Include complete ER records with readable copies of physician’s and nurse’s notes.
•Durable Medical Equipment: Complete description of the equipment and a valid HCPCS code, form or letter of medical necessity, detailed medical history, and approximate cost of the equipment.
•Ear, Nose and Throat: Office notes, operative notes, medical history, and the test results.
•Home Health Care: Physician notes, physician-signed treatment plan, and all notes for any services being performed by the agency.
•Inpatient Stays: Complete medical record.
•Laboratory: Patient history and lab results.
•Medical Care Issues: All office notes for the service in question. For cases involving denial of an office
visit/consultation and for any case involving the submission of Modifier 25: office notes, a patient history, reason for testing, and testing outcomes. If the case involves medication or administration of medication: office notes, and a detailed description of the medication, including dosage.
•MRI: The MRI report and a detailed patient history.
•Maternity: Detailed patient medical history, antenatal records, test results, labor and delivery records.
•Private Duty Nursing: Physician’s orders and all hourly nursing documentation.
•Podiatry: Operative reports and office notes for surgical cases, and lab/pathology reports.
•Radiology: The radiology report; medical history for PET scans.
•Skilled Nursing: All physician orders and progress notes, nursing notes, treatments, medication documentation, all therapy modalities, and any other relevant data.
•Surgery: Operative/procedure notes, and pathology reports (required) for cases involving the removal of lesions.
•Therapy: Progress notes; x-ray reports; re-exam findings; objective data, such as flow charts for any chiropractic, speech or occupational therapy service beyond the 10 treatments within a calendar year; and a completed Therapy Authorization form, located in the forms section of MedMutual.com.
•Transplant: In the Explanation field, a comprehensive problem statement.
•Vascular Services: Medical history and test results.
•Vision: Office notes, test results (if appropriate), and medical necessity information.
Claim Review: When the claim outcome varies from the benefits expected, for denial of services, for a
claim payment error, or reconsideration of a payment recovery (take back) or interest calculation. Requests for Claims Review will be returned unprocessed if submitted incorrectly.
•Duplicate Payment or Denial: When a duplicate claim payment was made or claims were erroneously denied as a duplicate in error.
•Requested Information Attached: Used for all claim denials related to the absence of data The
Company needs for final adjudication.
Type of Request continued
Page 3
•Pricing/UCR/APG/Outlier: When questioning the level of reimbursement. Examples include fee too low, not my agreed-to reimbursement rate, incorrect DRG, APG or Outlier Reimbursement. Claim copies are not needed.
•Timely Filing: Documentation that clearly shows The Company was in receipt of the claim (required).
Acceptable documentation includes a Company professional or hospital electronic claims Detail Accept/Reject Report, or fax receipt from The Company. Please note: Screen shots of Provider billings screens will not considered acceptable documentation for timely filing.
Please note: We will no longer accept PAR Forms for the following:
•COB: Requests related to the incorrect processing of COB or Medicare claims. [Note: If the original claim denied for another carrier’s EOB (E22) or Medicare’s EOB (MIM), it is not necessary to complete a PAR Form. Submit a new claim (electronic submission preferred) which includes the other carrier’s explanation of benefits information.]
•Corrected Billing: Must be submitted electronically using TOB XX5 or XX7.
When NOT to Use the PAR Form:
•Do not use the PAR Form if attempting to verify the status of a claim. Use the Provider ePortal, accessed through the Company website at Provider.MedMutual.com.
•Do not use the PAR Form if the claim has been returned unprocessed for additional data. Simply complete
the claim form with the additional or corrected data and resubmit the claim as a new claim electronically or by mailing it to:
Medical Mutual
P.O. Box 6018
Cleveland, Ohio 44101-1018
• Do not use a PAR Form to submit a late charge. Submit late charges electronically.
Additional Information
You may obtain a PAR Form by:
•Electronically submitting or printing out a copy of the PAR Form from the Company website:
Provider.MedMutual.com. The printable version must be used when submitting medical records or attachments with the PAR Form.
•Ordering printed copies. The PAR comes padded in quantities of 100 (Form number Z529). Fill out a
Supply Requisition Form (PC103). The Supply Requisition Form is located under Tools and Resources, Forms section of the Company’s website at Provider.MedMutual.com. Use pads as your quantity unit instead of individual forms when filling out your order. Either mail or fax the Supply Requisition Form to:
MZ: 18-5570 Inventory Control Medical Mutual
4601 Hinckley Industrial Parkway Cleveland, Ohio 44109-6020
Fax: (216) 687-7108 or (800) 677-8026
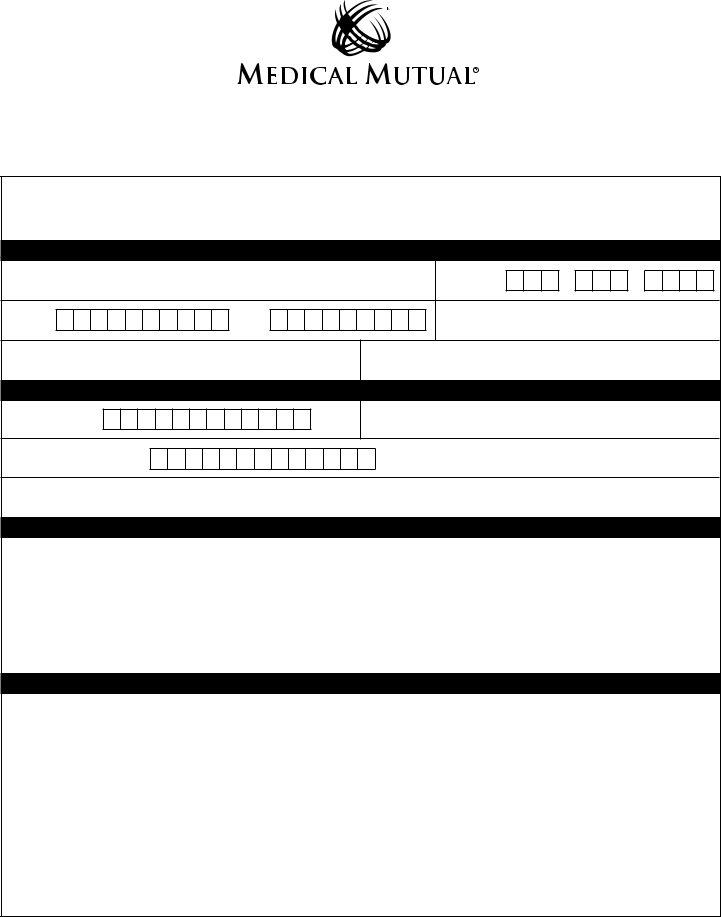
PROVIDER ACTION REQUEST (PAR) FORM
Fill out the form completely. Use one PAR form per patient. Requests submitted incomplete, incorrect, or with no PAR form will be returned unprocessed.
For quicker submission and faster processing, you can also fill out this form online. It is available on our website, Provider.Medmutual.com, in the Forms category under Tools & Resources. You can also access it online while you are viewing an ERA Statement in the logged-in portion of the website by clicking the Submit Inquiry button.
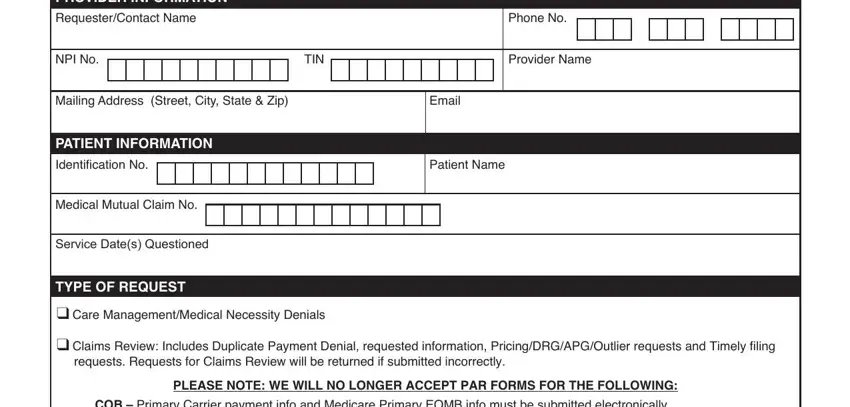
PROVIDER INFORMATION
Requester/Contact Name |
Phone No. |
Mailing Address (Street, City, State & Zip) |
Email |
PATIENT INFORMATION |
|
Identification No. |
Patient Name |
Medical Mutual Claim No.
SERVICE DATE(S) QUESTIONED
_______________________________________________________________________________________________________________
TYPE OF REQUEST geList Location in Directory?
q Care Management/Medical Necessity Denials
qClaims Review: Includes Duplicate Payment Denial, requested information, Pricing/DRG/APG/Outlier requests and Timely filing requests. Requests for Claims Review will be returned if submitted incorrectly.
PLEASE NOTE: WE WILL NO LONGER ACCEPT PAR FORMS FOR THE FOLLOWING:
COB – Primary Carrier payment info and Medicare Primary EOMB info must be submitted electronically. Corrected/Replacement Claim/Late Charges – Must be electronically submitted using TOB XX5 or XX7.
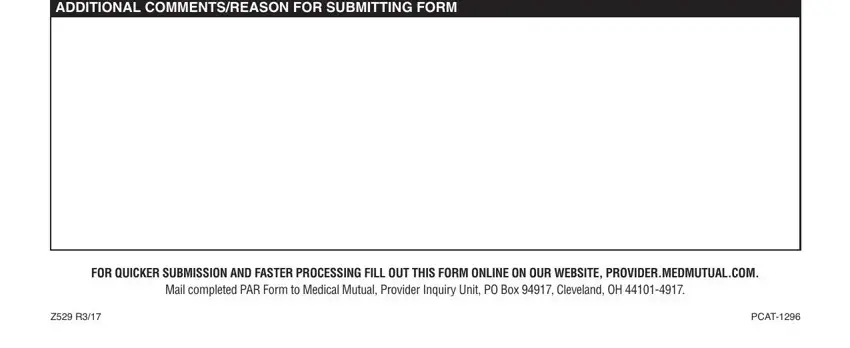
ADDITIONAL COMMENTS/REASON FOR SUBMITTING FORM
FOR QUICKER SUBMISSION AND FASTER PROCESSING FILL OUT THIS FORM ONLINE ON OUR WEBSITE, PROVIDER.MEDMUTUAL.COM.
Mail completed PAR Form to Medical Mutual, Provider Inquiry Unit, PO Box 94917, Cleveland, OH 44101-4917.