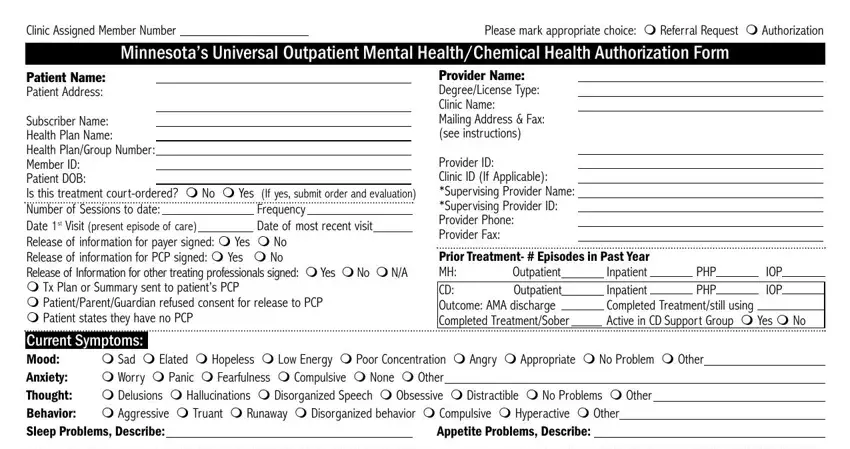
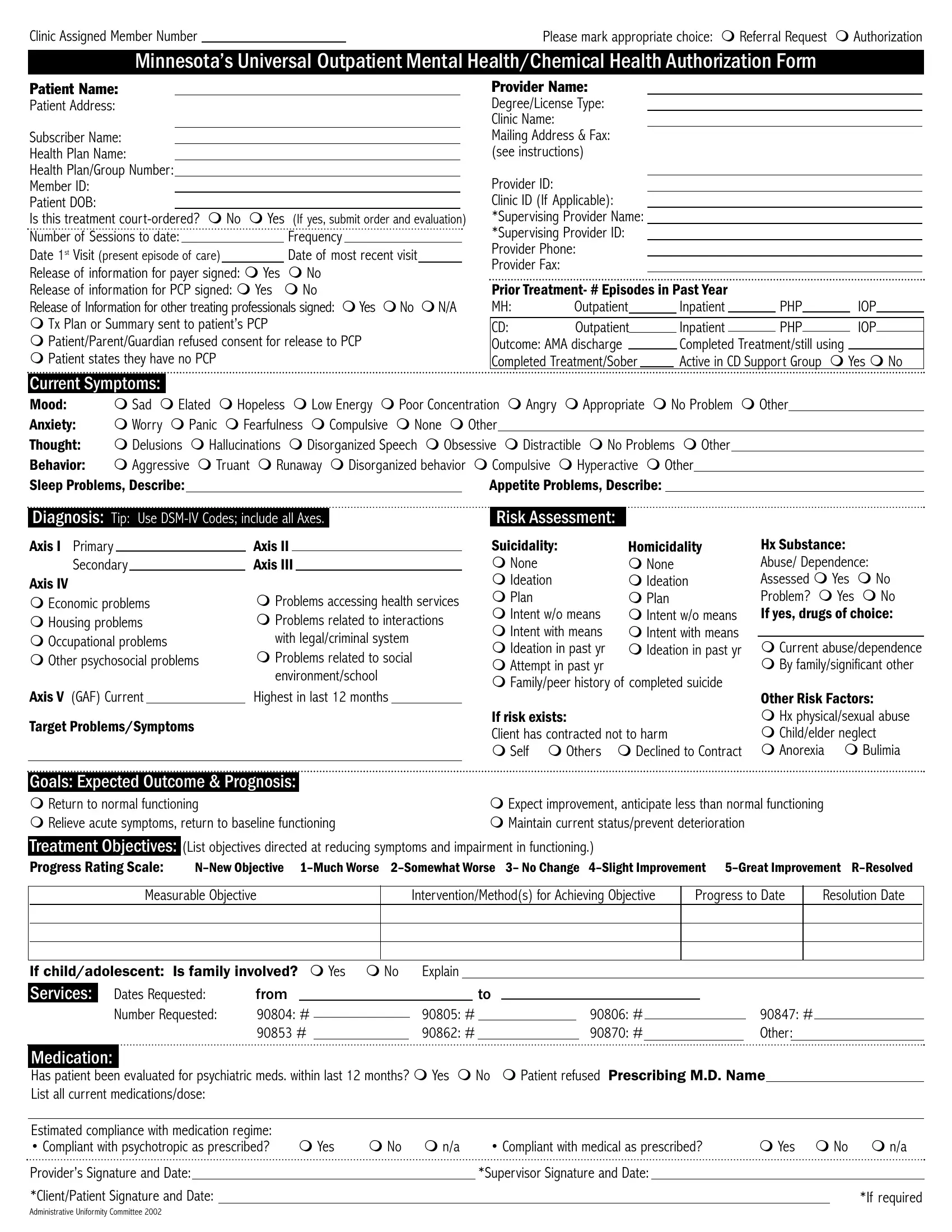
Clinic Assigned Member Number: This is an optional item that clinics/providers may use to record their internal account or reference number for the purpose of internally tracking submitted authorization forms.
Referral Request or Authorization Request: Check the appropriate box to indi- cate whether the document is being used to request authorization of services (including concurrent reviews for subsequent services) or to request a referral for services. A refer- ral request is generally a request submitted by an out-of-network provider who is request- ing that his/her services be covered under the patient's in-network benefits. Providers may need to check with the patient's health plan for specific requirements.
PATIENT/PROVIDER BLOCKS
Patient Address: Current address of patient, NOT subscriber's address. If the patient is a child who is in foster care, the patient address should reflect the foster care address.
Subscriber Name: Provide the name of the individual who is the subscriber of the insurance.
Health Plan Name: Provide the name of the health insurance company/plan.
Health Plan/Group Number: Provide the appropriate health plan/payer-assigned health plan or group number off of the patient's identification card.
Member ID: Provide the appropriate health plan/payer-assigned member identification number off of the patient's identification card.
Patient DOB: Provide the patient's date of birth.
Is this treatment court-ordered: Indicate whether the treatment is court-ordered and, if so, provide a copy of the order and the evaluation. The law requires that the health plan be given a copy of the court order and the behavioral care evaluation.
Provider Name: Provide the full name of the treating health care professional.
Degree/License Type: Provide the professional degree of the treating provider (e.g., M.D., Ph.D., Psy.D., M.S.W, M.A., R.N.); and provide the licensure type of the treating provider (e.g., LP, LICSW, LMFT, LACD, LPP).
Clinic Name: Provide the name of the clinic where the patient is being treated.
Mailing Address & Fax Number: Provide the mailing address, and a fax number, where authorizations/responses to this request should be sent. Note that this address may be different than the address where services will be provided.
Provider ID: Provide the appropriate health plan/payer-assigned provider identification number if available. Note that some health plans/payers may require this information to process this authorization request.
Clinic ID: Provide the appropriate health plan/payer-assigned clinic identification number where care is to be provided.
Supervising Provider Name: Provide the name of the supervising provider, if required for supervision or other appropriate circumstances.
Supervising Provider ID: Provide the health plan/payer-assigned provider identification number of the supervising provider, if required for supervision or other appropriate circum- stances.
Provider Phone: Provide a phone number for the treating provider.
Provider Fax: Provide a fax number for the treating provider.
Number of Sessions to Date/Frequency: Indicate the total number sessions, to date, that this patient has been seen by you/your clinic; and, indicate the frequency of those sessions (e.g., weekly, monthly, quarterly, etc.).
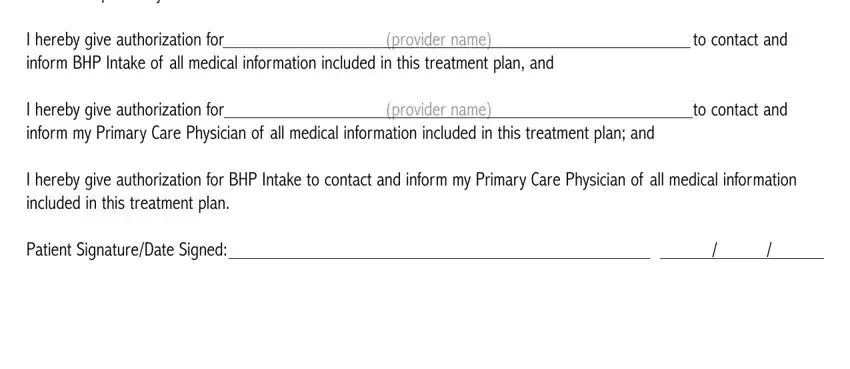
Release of Information for payer signed: Indicate whether the patient has signed a release of information form allowing information to be shared with his/her insurer/payer. Note that some health plans/payers (e.g., BHP) may have specific release of information requirements for initial requests. Providers may need to check with the patient's insurer/health plan for specific requirements.
Release of Information for PCP signed: Indicate whether the patient has signed a release of information form allowing information to be shared with his/her primary care provider (PCP). The attached release (page 2) is specifically required for BHP. Providers may need to check with the patient's insurer/health plan for other specific requirements.
Release of Information for other treating professionals signed: Indicate whether the patient has signed a release of information form allowing information to be shared with his/her other treating professionals. Providers may need to check with the patient's insurer/health plan for specific requirements.
Information Release Actions: Place a check mark before those statements that are true (TX plan or Summary sent to patient's PCP; Patient/Parent/Guardian refused consent for release to PCP; patient state they have no PCP).
Prior Treatment: If available, indicate for both mental health (MH) and chemical dependency (CD) treatment, the number of episodes of outpatient, inpatient, partial hospi- talization program (PHP), or intensive outpatient therapy (IOP) treatment provided in the past year.
CURRENT SYMPTOMS BLOCK
Identify the symptoms that the patient is currently experiencing. Attach additional sheet if nec- essary.
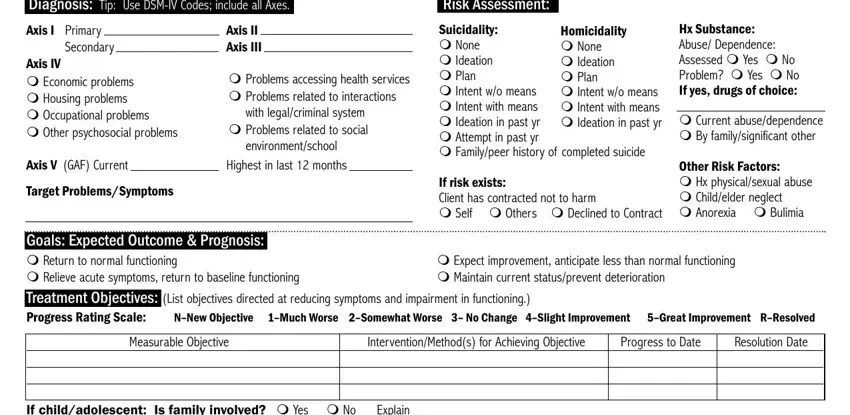
DIAGNOSIS BLOCK
Axis I: List the appropriate diagnosis code(s) for primary and secondary diagnoses, and other diagnoses as appropriate.
Axis II: List the appropriate diagnosis code(s).
Axis III: List the appropriate diagnosis code(s)
Axis IV: Identify patient stressors as appropriate.
Axis V (GAF): Provide the current GAF and the highest GAF within the last 12 months.
Target Problems/Symptoms: Summarize the patient's target problems/symptoms (attach additional sheet if necessary).
RISK ASSESSMENT BLOCK
Specify the patient's risk factors.
GOALS: EXPECTED OUTCOME & PROGNOSIS BLOCK
Indicate which of the four categories (return to normal functioning; relieve acute symptoms, return to baseline functioning; expect improvement, anticipate less than normal functioning; or, maintain current status/prevent deterioration) best describes the expected outcome and prognosis.
TREATMENT BLOCK
For each measurable objective identified (e.g., improve sleep patterns for three-five nights), identify the interventions/methods for achieving the objective (e.g., encourage exercise, provide and give instructions in use of sleep journal), the progress to date in achieving the objectives (using the progress rating scale provided), and the targeted resolution date.
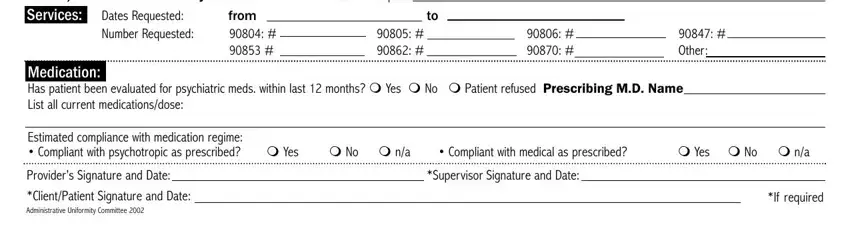
SERVICES BLOCK
Dates Requested: Indicate the range of dates for which services are being requested (from date and to date).
Number Requested: Provide the number of sessions/visits requested by procedure code. Requests for psychological testing, and any other services that are not listed under the codes provided, should be included on the "other" line with the appropriate service code.
MEDICATION BLOCK
Has patient been evaluated for psychiatric medication within last 12 months? Indicate whether the patient has been evaluated for psychiatric medication with- in the last 12 months, or if patient refused to respond.
Prescribing MD Name(s): Provide the name(s) of the prescribing physician(s) for patient's current medication(s).
Current Medications & Dosages: For initial requests, provide a list of all psy- chotropic and medical prescriptions, with dosages, the patient currently is using. For sub- sequent requests/reviews, list any changes to medications or dosages (attach additional sheet as necessary).
Estimated compliance with medication regime: Evaluate the patient's compli- ance with his/her medication regime for both psychotropic and medical prescriptions, as applicable.
Patient Signature: Obtain the patient's signature, if required. Note that some health plans/payers may require the patient's signature before authorization can be provided. Providers may need to check with the patient's health plan for specific requirements.