Aetna Transition of Care Coverage Questions and Answers
Q.What is Transition of Care (TOC) coverage?
A.TOC coverage is temporary coverage when you become a new member of an Aetna medical benefit plan or change your current Aetna medical plan, and a doctor you are being treated by:
•Is not in the Aetna network or;
•Leaves the Aetna network.
TOC coverage is not for Primary Care Physicians (PCPs) who are not in the Aetna network, except when the PCP leaves the Aetna network during your plan year, and you are receiving treatment, or if certain laws or regulations apply. TOC coverage allows a member who is receiving treatment to continue the treatment FOR A LIMITED TIME at the preferred plan benefit level. Approval of TOC requests are subject to the terms and limits of your plan. TOC coverage is only for the requested doctor and does not include facilities or hospitals. If the request is approved, the doctor must use a facility or hospital in the Aetna network.
QWhat0Bis an active course of treatment?
A. An active course of treatment is when you have begun a program of planned services with your doctor to correct or treat a diagnosed condition. The start date is the first date of service or treatment. An active course of treatment covers a certain number of services or period of treatment for special situations. Some examples may include, but are not limited to:
•Members enrolling with Aetna beyond 24 weeks of pregnancy (unless there are specific state or plan requirements). Members less than 24 weeks pregnant whom Aetna confirms as high risk are reviewed on a case-by-case basis.
•Members in an ongoing treatment plan, such as chemotherapy or radiation therapy;
•Members with a terminal illness, expected to live six months or less;
•Members who need more than one surgery, such as cleft palate repair;
•Members who have recently had surgery;
•Members who receive outpatient treatment for a mental illness or for substance abuse. (The member must have had at least one [1] treatment session within 30 days before the effective/renewal date of the Aetna plan).
•Members with an ongoing or disabling condition that suddenly gets worse;
•Members who may need or have had an organ or bone marrow transplant.
To be considered for TOC coverage, the course of treatment must have started before the enrollment or re-enrollment date or BEFORE the date your doctor left the Aetna network.
Q.What other types of providers, besides doctors, can be considered for TOC coverage?
A.Health care professionals such as physical therapists, occupational therapists, speech therapists, and agencies that provide skilled home care services such as visiting nurses. TOC does not apply to durable medical equipment (DME) vendors, health care facilities (e.g. hospital, skilled nursing facility) or pharmacy vendors.
Q.If I am currently receiving treatment from my doctor, why wouldn’t my request be approved for TOC coverage?
A.In addition to currently receiving treatment, your request must involve a covered procedure/service. Your doctor must also agree to accept the terms outlined on the TOC Request Form.
Q.How long does TOC coverage last?
A.Usually, TOC coverage lasts 90 days. You will be informed if your TOC coverage request is approved and how long it will last.
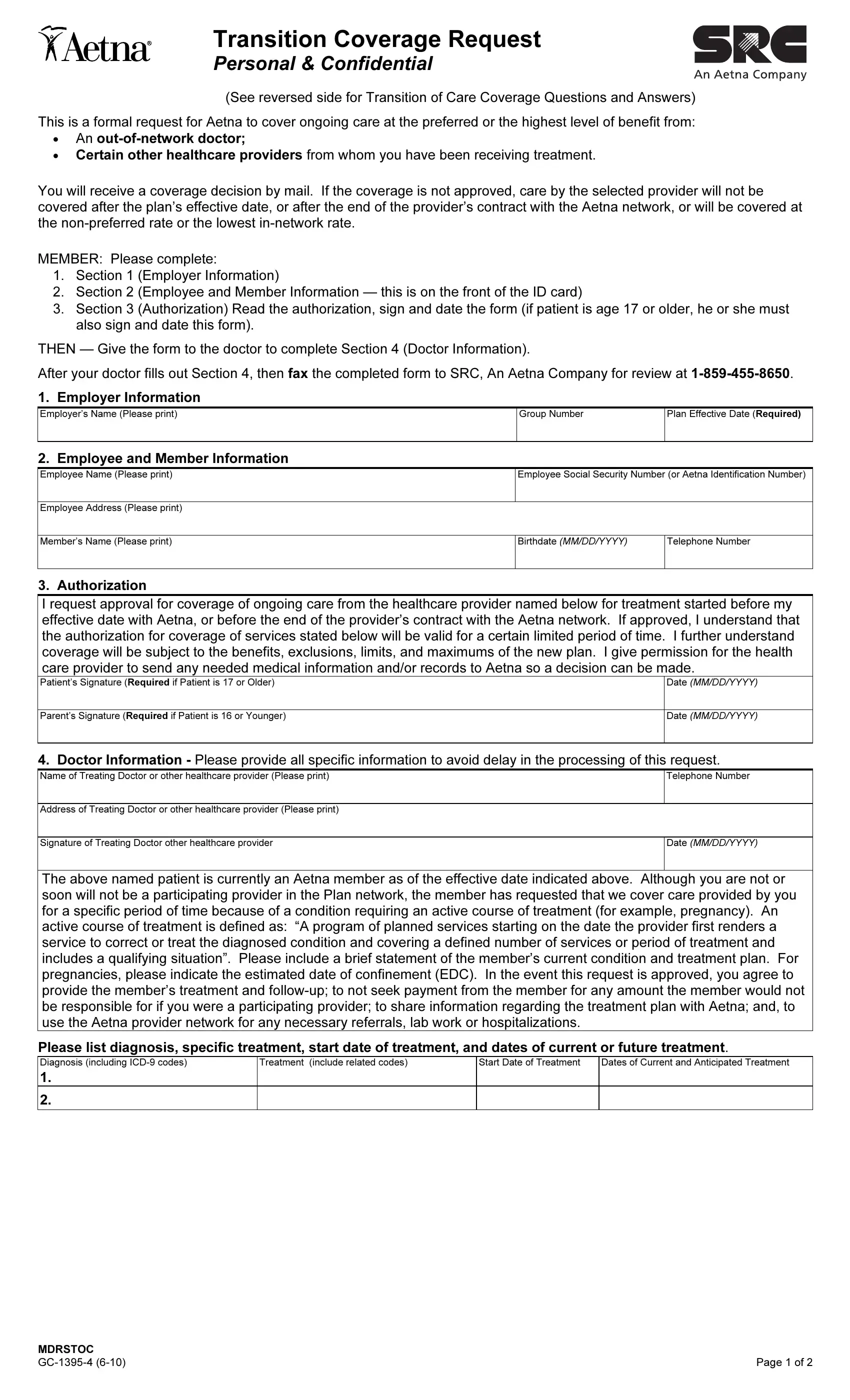
Q.How do I sign up for TOC coverage?
A.Contact1BMember Services. A TOC Request Form must be submitted to SRC:
•Within2Bninety (90) days of when you enroll or re-enroll; or
•Within3B90 days of the date, the provider left the Aetna network.
To4B get the highest level of benefit coverage, newly enrolling and re-enrolling members must be approved before receiving further services. You or your doctor can send in the request form.
Q.How will I know if my request for TOC coverage is approved?
A.You will receive a letter in the mail. The letter will say whether or not you are approved. If you are approved, any treatments you received before the approval date will not be covered at the highest benefit level, unless there was an emergency.
Q.I am going to receive services after the start date of my Aetna plan. The doctor is part of the Aetna network. Will the services be covered under my Aetna plan?
A.Please ask your doctor to confirm if approval is needed. If so, you can request approval by filling out a TOC form.
Misrepresentation
Any person who knowingly and with intent to injure, defraud or deceive any insurance company or other person files an application for insurance or statement of claim containing any materially false information or conceals, for the purpose of misleading, information concerning any fact material thereto commits a fraudulent insurance act, which is a crime and subjects such person to criminal and civil penalties.
Attention Arkansas, District of Columbia, Louisiana, Rhode Island and West Virginia Residents: Any person who knowingly presents a false or fraudulent claim for payment of a loss or benefit or knowingly presents false information in an application for insurance is guilty of a crime and may be subject to fines and confinement in prison. Attention California Residents: For your protection California law requires notice of the following to appear on this form: Any person who knowingly presents a false or fraudulent claim for the payment of a loss is guilty of a crime and may be subject to fines and confinement in state prison. Attention Colorado Residents: It is unlawful to knowingly provide false, incomplete, or misleading facts or information to an insurance company for the purpose of defrauding or attempting to defraud the company. Penalties may include imprisonment, fines, denial of insurance and civil damages. Any insurance company or agent of an insurance company who knowingly provides false, incomplete, or misleading facts or information to a policyholder or claimant for the purpose of defrauding or attempting to defraud the policyholder or claimant with regard to a settlement or award payable from insurance proceeds shall be reported to the Colorado division of insurance within the department of regulatory agencies. Attention Florida Residents: Any person who knowingly and with intent to injure, defraud, or deceive any insurer, files a statement of claim or an application containing any false, incomplete or misleading information is guilty of a felony of the third degree. Attention Kansas Residents: Any person who knowingly and with intent to injure, defraud or deceive any insurance company or other person submits an enrollment form for insurance or statement of claim containing any materially false information or conceals, for the purpose of misleading, information concerning any fact material thereto may have violated state law. Attention Kentucky Residents: Any person who knowingly and with intent to defraud any insurance company or other person files an application for insurance or statement of claim containing any materially false information or conceals, for the purpose of misleading, information concerning any fact material thereto commits a fraudulent insurance act, which is a crime and may subject such person to criminal and civil penalties. Attention Maine and Tennessee Residents: It is a crime to knowingly provide false, incomplete, or misleading information to an insurance company for the purpose of defrauding the company. Penalties may include imprisonment, fines, or denial of insurance benefits. Attention Maryland Residents: Any person who knowingly and willfully presents a false or fraudulent claim for payment of a loss or benefit or who knowingly and willfully presents false information in an application for insurance is guilty of a crime and may be subject to fines and confinement in prison. Attention New Jersey Residents: Any person who includes any false or misleading information on an application for an insurance policy or knowingly files a statement of claim containing any false or misleading information is subject to criminal and civil penalties. Attention New York Residents: Any person who knowingly and with intent to defraud any insurance company or other person files an application for insurance or statement of claim containing any materially false information, or conceals for the purpose of misleading, information concerning any fact material thereto, commits a fraudulent insurance act, which is a crime, and shall be subject to a civil penalty not to exceed five thousand dollars and the stated value of the claim for each violation. Attention North Carolina Residents: Any person who knowingly and with intent to injure, defraud or deceive any insurance company or other person files an application for insurance or statement of claim containing any materially false information or conceals, for the purpose of misleading, information concerning any fact material thereto commits a fraudulent insurance act, which may be a crime and subjects such person to criminal and civil penalties. Attention Ohio Residents: Any person who knowingly and with intent to defraud any insurance company or other person files an application for insurance or statement of claim containing any materially false information or conceals, for the purpose of misleading, information concerning any fact material thereto is guilty of insurance fraud. Attention Oklahoma Residents: WARNING: Any person who knowingly, and with intent to injure, defraud or deceive any insurer, makes any claim for the proceeds of an insurance policy containing any false, incomplete or misleading information is guilty of a felony. Attention Oregon Residents: Any person who with intent to injure, defraud, or deceive any insurance company or other person submits an enrollment form for insurance or statement of claim containing any materially false information or conceals for the purpose of misleading, information concerning any fact material thereto may have violated state law. Attention Pennsylvania Residents: Any person who knowingly and with intent to defraud any insurance company or other person files an application for insurance or statement of claim containing any materially false information or conceals, for the purpose of misleading, information concerning any fact material thereto commits a fraudulent insurance act, which is a crime and subjects such person to criminal and civil penalties. Attention Puerto Rico Residents: Any person who knowingly and with the intention to defraud includes false information in an application for insurance or file, assist or abet in the filing of a fraudulent claim to obtain payment of a loss or other benefit, or files more than one claim for the same loss or damage, commits a felony and if found guilty shall be punished for each violation with a fine of no less than five thousand dollars ($5,000), not to exceed ten thousand dollars ($10,000); or imprisoned for a fixed term of three (3) years, or both. If aggravating circumstances exist, the fixed jail term may be increased to a maximum of five
(5)years; and if mitigating circumstances are present, the jail term may be reduced to a minimum of two (2) years. Attention Vermont Residents: Any person who knowingly and with intent to injure, defraud or deceive any insurance company or other person files an application for insurance or statement of claim containing any materially false information or conceals, for the purpose of misleading, information concerning any fact material thereto commits a fraudulent insurance act, which may be a crime and may subject such person to criminal and civil penalties. Attention Virginia Residents: Any person who knowingly and with intent to injure, defraud or deceive any insurance company or other person files an application for insurance or statement of claim containing any materially false information or conceals, for the purpose of misleading, information concerning any fact material thereto commits a fraudulent act, which is a crime and subjects such person to criminal and civil penalties. Attention Washington Residents: It is a crime to knowingly provide false, incomplete, or misleading information to an insurance company for the purpose of defrauding the company. Penalties include imprisonment, fines, and denial of insurance benefits.