We used the top-rated computer programmers to implement this PDF editor. This app will help you fill out the blue view vision form document easily and won't require a lot of your energy. This simple instruction will assist you to start out.
Step 1: Click the "Get Form Here" button.
Step 2: Now you are on the form editing page. You may change and add content to the form, highlight words and phrases, cross or check particular words, include images, put a signature on it, delete unneeded areas, or take them out altogether.
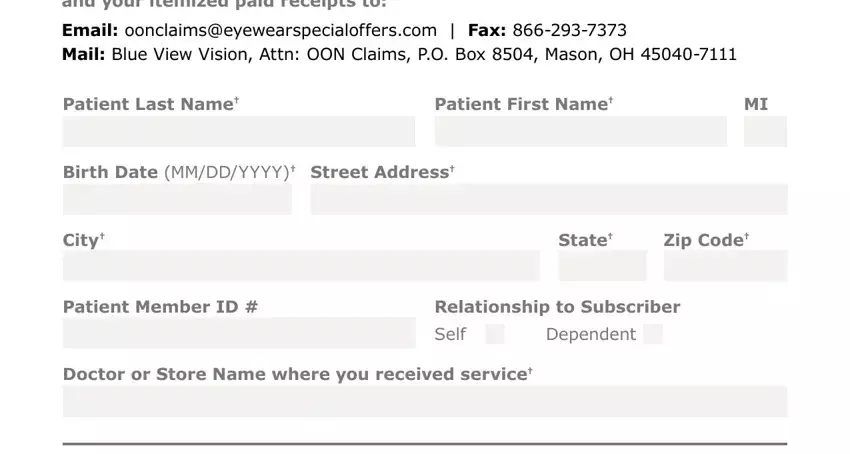
The following areas are what you will have to complete to get the finished PDF form.
Please note the crucial details in the Patient, LastName Patient, First, Name BirthDate, MM, DD, YYYY, Street, Address City, State, Zip, Code Patient, Member, ID Relationship, to, Subscriber, Self and Dependent field.
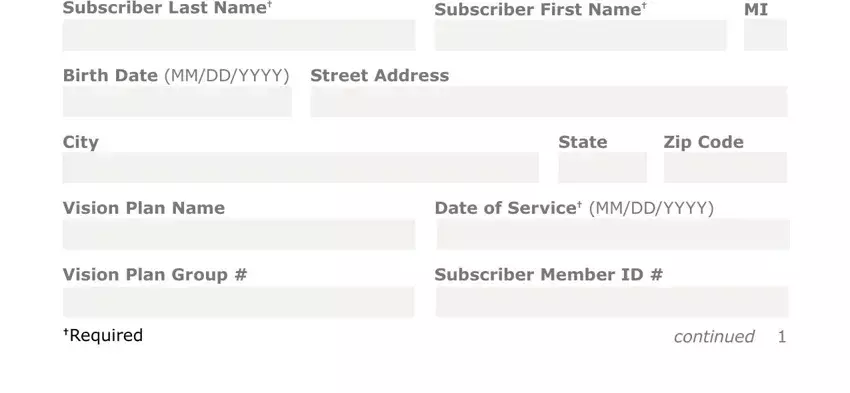
You'll be required certain key information to fill out the Subscriber, LastName Subscriber, First, Name BirthDate, MM, DD, YYYY Street, Address City, State, Zip, Code Vision, Plan, Name Date, of, Service, MM, DD, YYYY Vision, Plan, Group Subscriber, Member, ID and Required box.
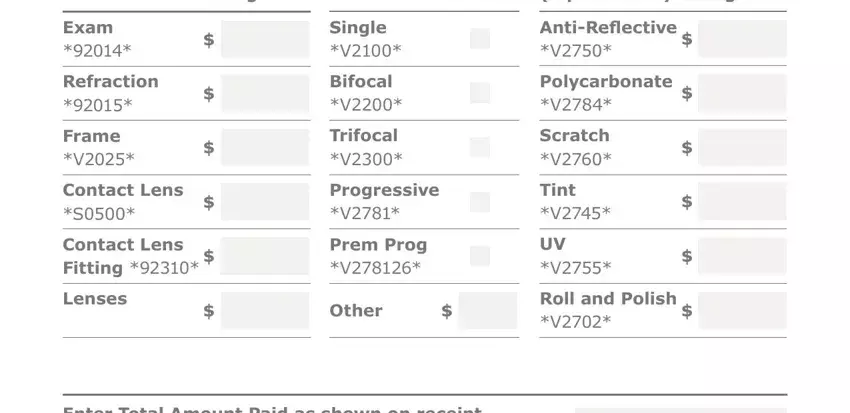
Describe the rights and obligations of the sides within the field Amount, Charged Please, Check Lens, Options, if, purchased Amount, Charged and Other.
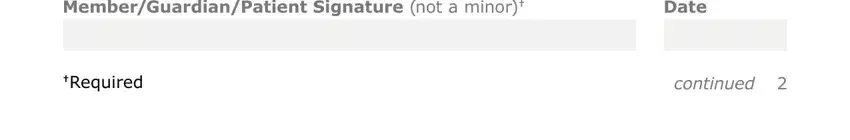
Finish the form by reading all of these fields: Date, and Required.
Step 3: Once you pick the Done button, the completed file is simply transferable to every of your gadgets. Or alternatively, you might send it by means of mail.
Step 4: Create a copy of every different file. It will save you some time and permit you to refrain from challenges in the future. By the way, your data isn't revealed or monitored by us.