DNR Order Form
A do not resuscitate order is a healthcare document that has serious ramifications. A person signing this document instructs the healthcare professionals, whether at a hospice or at a hospital, not to conduct CPR on them. This includes both mild methods like chest compressions and more advanced methods like using a defibrillator or inserting a tube to assist breathing. Ultimately, a DNR form forbids any form of cardiopulmonary resuscitation to allow natural death.
There are countless reasons why a person would sign that kind of an order, from the understanding that their illness will not let them live long after the resuscitation to various religious beliefs. Regardless of your reason, you might want to create a do not resuscitate (DNR) form to let your decisions known.
Consult with your doctor if needed, inform your relatives or healthcare proxy about your decision, and sign the form. That will make sure the doctors do not act against your decision and attempt resuscitation.
Here, you will find everything you need to sign a DNR order from more information on what it is and how it works to a free DNR form. You can download it, print it, and fill it out to attach it to your medical record.
Build Your Document
Answer a few simple questions to make your document in minutes
Save and Print
Save progress and finish on any device, download and print anytime
Sign and Use
Your valid, lawyer-approved document is ready
What is a DNR (Do Not Resuscitate) order form?
A DNR order or a do not resuscitate order is a legal document that is created to make sure the doctors do not attempt resuscitation on the person who signed it. It’s also known as the do not attempt to resuscitate (DNAR) order and may include a DNI (do not intubate order), although this is a different order from the do not resuscitate order (DNR).
Since resuscitation methods are now more advanced than CPR, some states interpret the do not resuscitate order as relating to cardiopulmonary resuscitation only. In such a case, the order is also known as “No CPR.”
It’s a common misconception that if you have a tattoo that says “do not resuscitate,” the healthcare professionals will not attempt resuscitation.
If a patient’s heart stops beating, they stop breathing, or their blood flow stops, the medics will conduct cardiopulmonary resuscitation (CPR) unless there’s a yellow form attached to their papers. A tattoo, a bracelet, or DNR jewelry will only guide them to look for such an order, but it’s not legally binding in any way.
In some countries, it’s possible to order your doctors not to attempt resuscitation orally, but in the US it’s not enough. The patient may reinforce the order orally, but they do need to have a do not resuscitate (DNR) form signed for that to be legally binding.
A DNR form can be signed in the hospital by the patient or their health care proxy, but some states put significant strains on that to prevent misuse of the order. This is why it’s always a good idea to sign an out-of-hospital DNR form.
They do not attempt resuscitation orders does not imply there should be less care for the patient. It only instructs the medics to not resuscitate the patient with the help of CPR. All the other forms of treatment like life support procedures, pain medications, etc. are permitted.
In practice, however, patients who sign a DNR form often decide to request less care overall. This may be due to a terminal illness or other condition that would only worsen should the patient’s life be prolonged with the wonders of modern medicine. If that is your case, you would need more than a DNR form.
You can find other medical-legal documents detailing end-of-life decisions and how do they differ from the DNR below.
Disambiguations regarding DNR form
DNR vs living will
A do not resuscitate order and a living will are different documents that give healthcare professionals instructions on end-of-life decisions. Even though they’re often signed together, they have very different scopes.
A DNR form indicates that the patient does not want to receive CPR. In the case of respiratory arrest or heart failure, the patient will not be resuscitated. This includes basic methods like cardiac massage or more advanced methods like defibrillation that delivers an electric shock to the heart.
A living will have a much wider scope. It details what types of life support a patient wishes to receive. This goes far beyond cardiopulmonary resuscitation alone. The living will include:
- General life support decisions
- Feeding tube
- Intravenous feeding
- Dialysis
- Lung ventilation
- Intubation
- Organ donation
- Donating brain and other organs to medical research after the demise
DNR vs advance directive
An advance directive or advance healthcare directive is an umbrella term that may cover the DNR order as well as other documents that cover end-of-life health care decisions. Both the order to not resuscitate and living will be considered a part of the advance directive.
The thing that combines them is that they continue being legally binding after the patient is able to consent or communicate. This makes durable medical power of attorney form a part of an advance healthcare directive, but non-durable POAs are exempt.
DNR vs full code
DNR order and full code are completely opposite things. If the patient’s card does not have a DNR order, their status in the emergency room is considered “full code.” This means the primary care physician will attempt anything necessary to bring them back should they suffer a cardiac arrest. Under full code, the health care providers will attempt any measure from cardiac massage to lung intubation to assist breathing before the patient is brought back to life.
With a DNR order in place, the patient’s status is considered to be “no code.” The medics will know not to attempt any of these measures and will allow natural death.
POLST vs DNR
Physician Orders for Life-Sustaining Treatment or POLST is a legal document that can complement the advance directive, but only for some patients. It’s only applicable if the patient was diagnosed with a terminal illness or frailty from old age. As these conditions will only worsen the patient’s state and lead to suffering, they may want to sign this form to direct their healthcare professionals on their end-of-life decisions.
Also known as Medical Orders for Life-Sustaining Treatment (MOLST), it directs the healthcare professionals to provide ordinary measures that ease the burden on the patient but withhold more serious life support measures.
When is a DNR order appropriate?
Taking a decision to not receive resuscitation in case of a cardiac arrest is not something you take lightly. This is why most adults are discouraged from signing a DNR order and it can only be signed after a consultation with a physician. Here is why someone would sign a do not resuscitate order.
- They have a long-term illness with no signs of improvement
- They are in prolonged severe pain such as from late-stage cancer
- They are terminally ill and CPR will only prolong the suffering
- They have an illness that impacts the quality of life like dementia or Alzheimer’s disease
- They are unlikely to survive CPR due to illness or old age
- They are in a hospice, nursing home, or another type of end-of-life care facility
Do Not Resuscitate (DNR) Order Laws by State
| STATES | SIGNING REQUIREMENTS | STATE LAW |
| Alabama | Patient & Physician | Alabama Administrative Code, Section 420-5-19-.02 |
| Alaska | Patient & Physician | Alaska Statutes, Section 13.52.160 |
| Arizona | Patient, Physician & Witness | Arizona Revised Statutes, Section 36-3251 |
| Arkansas | Patient & Physician | Arkansas Annotated Code, Sections 20-13-901 to 20-13-908 |
| California | Patient & Physician | California Probate Code, Section 4780 |
| Colorado | Patient & Physician | Colorado Revised Statutes, Section 15-18.6-102 |
| Connecticut | Patient & Physician | Connecticut Revised Statutes, Chapter 368w, Section 19a-580d |
| Delaware | Patient & Physician | Delaware Code, Title 16, Section 2509A |
| Florida | Patient & Physician | Florida Administrative Code, Section 64J-2.018 |
| Georgia | Physician | Georgia Code, Sections 31-39-2 to 31-39-9 |
| Hawaii | Patient & Physician | Hawaii Revised Statutes, Section 327K-2 |
| Idaho | Patient & Physician | Idaho Statutes, Section 39-4514 |
| Illinois | Patient, Physician & Witness | Illinois Compiled Statutes, Chapter 755, Section 40/65 |
| Indiana | Patient, Physician & Two Witnesses | Indiana Code, Sections 16-36-5-1 to 16-36-5-28 |
| Iowa | Physician | Iowa Code, Section 144A.7A |
| Kansas | Patient, Physician & Witness | Kansas Statute, Section 65-4943 |
| Kentucky | Patient & Two Witnesses OR Notary Public | Kentucky Revised Statutes, Section 311.623 |
| Louisiana | Patient & Physician | Louisiana Revised Statutes, Section 40:1155.3 |
| Maine | Patient & Physician | Maine Revised Statutes, Title 32, Section 93-A.1(b) |
| Maryland | Physician | Maryland Annotated Code, Section 5-608.1 |
| Massachusetts | Patient & Physician | – |
| Michigan | Patient, Physician & Two Witnesses | Michigan Compiled Laws, Section 333.1053 |
| Minnesota | Patient & Physician | Minnesota Statutes, Chapter 145C |
| Mississippi | Patient & Physician | Mississippi Annotated Code, Section 41-41-302 |
| Missouri | Patient & Physician | Missouri Revised Statutes, Section 190.603 |
| Montana | Patient & Physician | Montana Public Health and Human Services, Chapter 37.10 |
| Nebraska | Patient, Physician & Witness for DNR; Patient & Two Witnesses OR Notary Public for Declaration | Nebraska Revised Statutes, Section 20-404 |
| Nevada | Patient & Physician | Nevada Revised Statutes, Section 450B.520 |
| New Hampshire | Patient & Physician | New Hampshire Revised Statutes, Section 137-J:26 |
| New Jersey | Patient & Physician | New Jersey Administrative Code, Section 10:48B |
| New Mexico | Patient & Physician | New Mexico Administrative Code, Section 7.27.6.8 |
| New York | Patient & Physician | New York Senate Bill S7883 |
| North Carolina | Patient & Physician for MOST; Patient, Two Witnesses & Notary Public for Declaration | North Carolina General Statutes, Sections 90-321 and 90-322 |
| North Dakota | Patient & Physician for POLST | North Dakota Century Code, Chapter 23-06.5 |
| Ohio | Physician | Ohio Administrative Code, Chapter 3701-62 |
| Oklahoma | Patient, Physician & Two Witnesses | Oklahoma Statutes, Section 63-3131.5 |
| Oregon | Physician for POLST | Oregon Administrative Rules, Sections 847-035-0030(6) and 847-010-0110 |
| Pennsylvania | Patient & Physician | Pennsylvania Consolidated Statutes, Title 20, Sections 5481-5488 |
| Rhode Island | Patient & Physician | Rhode Island General Laws, Chapter 23-4.11 |
| South Carolina | Patient & Physician | South Carolina Code of Laws, Sections 44-78-10 to 44-78-65 |
| South Dakota | Patient & Physician | South Dakota Administrative Rules, Chapter 44:05:06; Codified Laws, Chapter 34-12F |
| Tennessee | Patient & Physician for POST | Tennessee Code Annotated, Section 68-11-224 |
| Texas | Patient, Physician & Two Witnesses OR 2nd Physician | Texas Statutes, Health and Safety Code, Chapter 166; Administrative Code, Rule 157.25 |
| Utah | Patient & Physician (2nd Physician is Required for Minors) | Utah Administrative Rules, Section R432-31 |
| Vermont | Patient (if able to sign) & Physician | Vermont Statutes, Title 18, Sections 9708 and 9709 |
| Virginia | Patient & Physician | Virginia Code, Section 54.1-2987.1 |
| Washington | Patient & Physician for POLST | Washington Revised Code, Section 43.70.480; Chapter 70.245 |
| West Virginia | Patient & Physician for POST | West Virginia Code, Chapter 16-30C |
| Wisconsin | Patient & Physician | Wisconsin Statutes and Annotations, Sections 154.17-154.29 |
| Wyoming | Patient & Physician | Wyoming Statutes, Sections 35-22-501 to 35-22-509 |
How to get a Do Not Resuscitate order?
text Make sure to create general actionable steps that a person should take to get a DNR. You can use the images from the first website-example as a reference.
Talk to your doctor
You need your practicing physician to co-sign the DNR form. But even apart from that requirement, you should talk to your doctor first before signing the form. This will make sure you are fully aware of what this decision means for your well-being.
Download a DNR form
The next step is to download a DNR form to fill out. You can find one free of charge here at SITENAME. Make sure you print it on yellow paper as it’s required by law in most states.
Invite two witnesses
Some states require the form to be notarized, but in most places, you will be able to have two witnesses over to co-sign it. Invite the witnesses and complete the signing with them.
Fill it in and sign it
The next step is fairly easy. Put your name on the document, fill in the date, and sign the document. Let the witnesses sign it as well.
It also requires authorization from your physician. They should put their name and signature on the document.
Send the copies
The primary care physicians who are taking care of you in an emergency situation may rush to save your life above all else. This is why it’s important to make sure that every person who is involved in health care knows there’s a DNR order. This includes the health care team, but you may also send copies to your health care proxy, and your loved ones if needed.
Display the DNR form (optional)
Some people want to make sure that their decisions are honored, especially in a rush that ensues after a cardiac arrest. This is why it may be a good idea to have a way to cue the medical personnel you have signed a DNR. Display it in your home or wear a wristband to let the first responders know they should contact your physician and verify there is a DNR order.
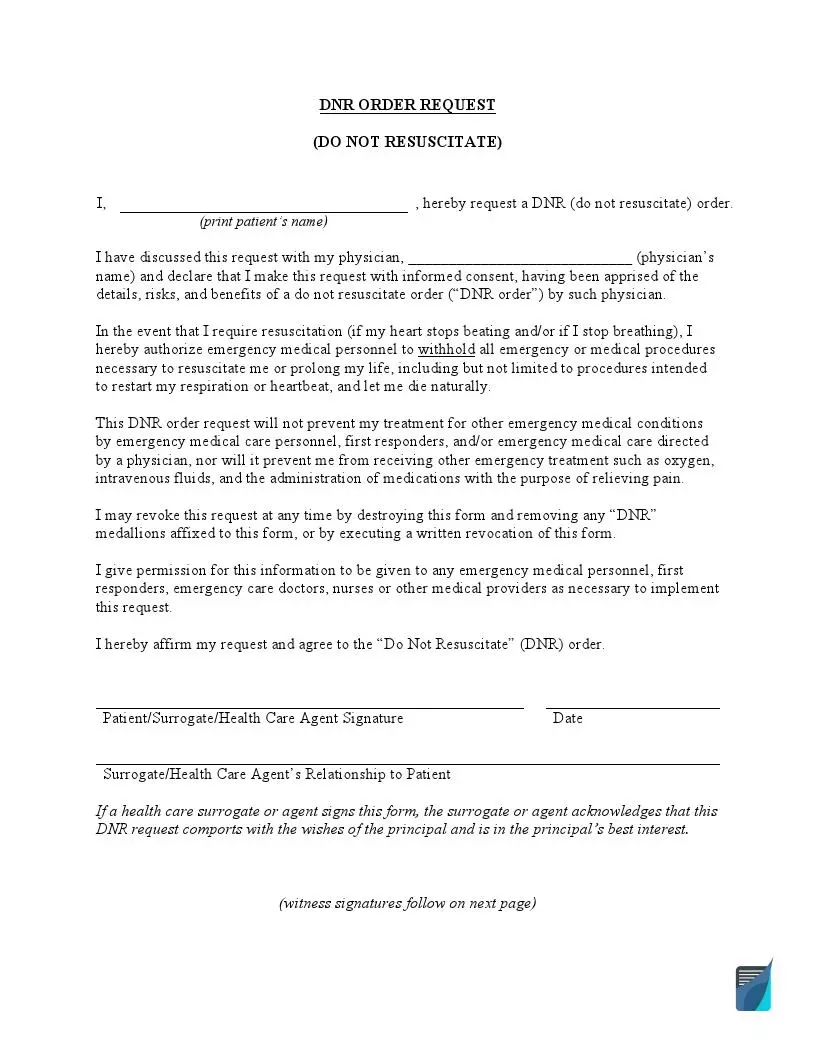
Download a free DNR order form
A do not resuscitate order is a fairly easy document to fill in, but before you can do that, you’ll need sample DNR forms that are viable in multiple states. You can download a free DNR order here on SITENAME.
Make sure you check with your physician and print it on yellow paper as it is required in most states.
How to Create a DNR order? (Filling Guide)
Once you download the DNR form, it’s actually easy to fill in. Here are all the steps that you need to go through.
Fill in your name and sign the document
Other than understanding all the legal ramifications of the DNR form, there isn’t much to fill in. Put your name and signature on the document in front of two witnesses and a physician and let them continue.
In some situations, like the patient being unable to communicate, their medical attorneys may sign the document in their name. In this case, they should sign a medical POA form beforehand and give the individuals who will act in your stead the said powers.
Let your physician sign the document
Since a do not resuscitate order has serious ramifications for your health, the proper procedure is to have it co-signed by a doctor. Start by putting their name on the form in the appropriate field.
The document also has a special section that should be filled by your physician. Let them sign the document and proceed.
Let two witnesses or a notary sign the document
The last part is giving the document to the two witnesses to co-sign. Most states require either a witness or a notary to sign the document for it to obtain legal power. If you do not have two witnesses, to co-sign, you can use the services of a notary public to make the document legal.
Once they sign the notary acknowledgment section, the document gains legal power.
Frequently Asked Questions
What will happen if I don't write a DNR?
If you wish not to be resuscitated and do not write a DNR order, your status in primary care will be full code. This means the emergency medical personnel will do anything necessary to bring you back to life, even if it means survivability after that is questionable.
No tattoos or bracelets alone are enough to put yours legally into the code status. You do need a DNR order for that. If you only have the DNR form, however, the healthcare providers will attempt other treatments.
Can a DNR be revoked?
Yes, a DNR order can be revoked at any time. The patient, their medical attorney, or their physician may reassess and revoke the DNR form. To do this, according to laws in most states, they have to fill in the revocation of the DNR form, inform all medical staff about this, obtain all existing copies of a DNR form, and mark them with a bold black X. The original should be destroyed.
What makes a DNR valid?
To make a DNR form valid, you need your physician and two witnesses to co-sign the document. Once they put their names and signatures in the appropriate section of the document, it gains power.
What happens if DNR is not followed?
Dealing with a patient who suffered cardiac arrest and has a DNR form may be tricky since from the point of view of ethics, the medics have to save everyone. Legally speaking, if it happens out of the hospital, the first responders are obligated to do everything they can to save that person. If they didn’t know there’s a DNR order, they may not be held responsible.
If it happens in the hospital, however, it’s quite a different story. The staff is obligated to ask for DNR orders and follow them. Otherwise, they will be held legally responsible.
Is it possible to create a DNR without a patient's consent?
Creating a DNR form requires the consent of the patient either directly or via proxy. Even though the health care surrogate may sign the DNR form for the patient who is incapacitated, it can only be done if the patient gave them those powers.
How to get a DNR if a patient and their family disagree?
It may be tough for the family, but the decision on the DNR form is made between the patient and their physician. Relatives disagreeing on what’s the best course of action is not a reason not to get a DNR form. Only the patient has the right to make decisions about their health care.
The only way a DNR form can be refused to a patient in need is if they show signs of depression or cannot fully comprehend the treatment options if they’re not of sound mind.